Health Library
Omphalocele
Birth defect - omphalocele; Abdominal wall defect - infant; Abdominal wall defect - neonate; Abdominal wall defect - newborn
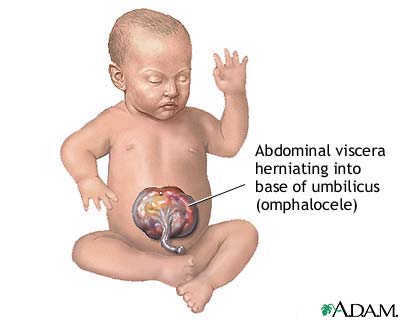
An omphalocele is a birth defect in which an infant's intestine or other abdominal organs are outside of the body because of a hole in the belly button (navel) area. The intestines are covered only by a thin layer of tissue and can be easily seen.
Images

Presentation

I Would Like to Learn About:
Causes
An omphalocele is considered an abdominal wall defect (a hole in the abdominal wall). The child's intestines usually stick out (protrude) through the hole.
The condition looks similar to gastroschisis. An omphalocele is a birth defect in which the infant's intestine or other abdominal organs protrude through a hole in the belly button area and are covered with a membrane. In gastroschisis, there is no covering membrane.
Abdominal wall defects develop as a baby grows inside the mother's womb. During development, the intestines and other organs (liver, bladder, stomach, and ovaries or testes) develop outside the body at first and then usually return inside. In babies with omphalocele, the intestines and other organs remain outside the abdominal wall, with a membrane covering them. The exact cause for abdominal wall defects is not known.
Infants with an omphalocele often have other birth defects. Defects include genetic problems (chromosomal abnormalities), congenital diaphragmatic hernia, and heart and kidney defects. These problems also affect the overall outlook (prognosis) for the baby's health and survival.
Symptoms
An omphalocele can be clearly seen. This is because the abdominal contents stick out through the belly button area.
There are different sizes of omphaloceles. In small ones, only the intestines remain outside the body. In larger ones, the liver or other organs may be outside as well.
Exams and Tests
Prenatal ultrasounds often identify infants with an omphalocele before birth, usually by 20 weeks of pregnancy.
Testing is often not necessary to diagnose omphalocele. However, babies with an omphalocele should be tested for other problems that often go with it. This includes ultrasounds of the kidneys and heart, and blood tests for genetic disorders, among other tests.
Treatment
Omphaloceles are repaired with surgery, although not always immediately. A sac protects the abdominal contents and may allow time for other more serious problems (such as heart defects) to be dealt with first, if necessary.
Some smaller omphaloceles can be closed immediately by surgery. To close a larger omphalocele, the sac is covered with a sterile mesh material, which is then stitched in place to form what is called a silo. As the baby grows over time, the abdominal contents are pushed into the abdomen by gravity.
When the omphalocele can comfortably fit within the abdominal cavity, the silo is removed and the abdomen is closed.
Because of the pressure involved in returning the intestines to the abdomen, the baby may need support to breathe with a ventilator. Other treatments for the baby include nutrients by IV and antibiotics to prevent infection. Even after the defect is closed, IV nutrition will continue as milk feedings must be introduced slowly.
Sometimes an omphalocele is so large that it cannot be placed back inside the infant's abdomen. The skin around the omphalocele grows and eventually covers the omphalocele. The abdominal muscles and skin can be repaired when the child is older for a better cosmetic outcome.
Outlook (Prognosis)
Complete recovery is expected after surgery for an omphalocele. However, omphaloceles often occur with other birth defects. How well a child does will depend on which other conditions the child has.
If the omphalocele is identified before birth, the mother should be closely monitored to make sure the unborn baby remains healthy.
Plans should be made for careful delivery and immediate management of the problem after birth. The baby should be delivered in a medical center that is skilled at repairing abdominal wall defects. Babies are likely to do better if they do not need to be taken to another center for further treatment.
Parents should consider testing the baby, and possibly family members, for other genetic problems that are associated with this condition.
Possible Complications
The increased pressure from the misplaced abdominal contents can decrease blood flow to the intestine and kidneys. It can also make it difficult for the baby's lungs to expand, leading to breathing problems.
Another complication is bowel death leading to necrosis of the bowel. This occurs when intestinal tissue dies due to low blood flow or infection. The risk may be reduced in babies who receive maternal milk rather than formula.
When to Contact a Medical Professional
This condition is apparent at birth and will be detected in the hospital at delivery if it has not already been seen on routine fetal ultrasound exams during pregnancy. If you have given birth at home and your baby appears to have this defect, call 911 or the local emergency number right away.
This problem is diagnosed and repaired in the hospital at birth. After returning home, call your health care provider if your baby develops any of these symptoms:
- Decreased bowel movements
- Feeding problems
- Fever
- Green or yellowish green vomit
- Swollen belly area
- Vomiting (different than normal baby spit-up)
- Worrisome behavioral changes
Related Information
Umbilical herniaGastroschisis
Omphalocele repair
References
Centers for Disease Control and Prevention website. Birth defects. Omphalocele. www.cdc.gov/birth-defects/about/omphalocele.html. Updated May 16, 2024. Accessed June 18, 2024.
Islam S. Congenital abdominal wall defects: gastroschisis and omphalocele. In: Holcomb GW, Murphy JP, St. Peter SD, eds. Holcomb and Ashcraft's Pediatric Surgery. 7th ed. Philadelphia, PA: Elsevier; 2020:chap 48.
Polites S, Nathan JD. Newborn abdominal wall defects. In: Wyllie R, Hyams JS, Kay M, eds. Pediatric Gastrointestinal and Liver Disease. 6th ed. Philadelphia, PA: Elsevier; 2021:chap 58.
BACK TO TOPReview Date: 12/31/2023
Reviewed By: Mary J. Terrell, MD, IBCLC, Neonatologist, Cape Fear Valley Medical Center, Fayetteville, NC. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
