Health Library
Nipple discharge
Discharge from breasts; Milk secretions; Lactation - abnormal; Witch's milk (neonatal milk); Galactorrhea; Inverted nipple; Nipple problems; Breast cancer - discharge
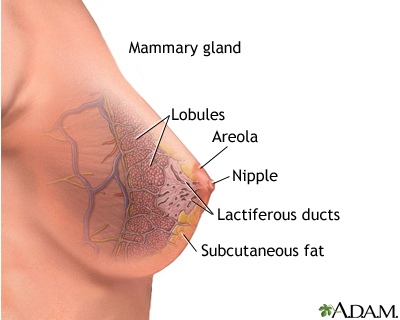
Nipple discharge is any fluid that comes out of the nipple area in your breast.
Images




I Would Like to Learn About:
Causes
Sometimes discharge from your nipples is OK and will get better on its own. You are more likely to have nipple discharge if you have been pregnant at least once.
Nipple discharge is most often not due to cancer, but rarely, it can be a sign of breast cancer. It is important to find out what is causing it and to get treatment. Here are some reasons for nipple discharge:
- Pregnancy
- Recent breastfeeding
- Rubbing on the area from a bra or t-shirt
- Injury to the breast
- Breast infection
- Inflammation and clogging of the breast ducts
- Noncancerous pituitary tumors
- Small growth in the breast that is usually not cancer
- Severe underactive thyroid gland (hypothyroidism)
- Fibrocystic breast (normal lumpiness in the breast)
- Use of certain medicines, such as birth control pills or antidepressants
- Use of certain herbs, such as anise, blessed thistle, and fennel
- Widening of the milk ducts
- Intraductal papilloma (benign tumor in the milk duct)
- Chronic kidney disease
- Illicit drug use, including cocaine, opioids and marijuana
Sometimes, babies can have nipple discharge. This is caused by hormones from the mother before birth. It should go away in 2 weeks.
Cancers such as Paget disease (a rare type of cancer involving the skin of the nipple) can also cause nipple discharge.
Symptoms
Nipple discharge that is not normal is:
- Bloody
- Comes from only one nipple
- Comes out on its own without you squeezing or touching your nipple
Nipple discharge is more likely to be normal if it:
- Comes out of both nipples
- Happens when you squeeze your nipples
The color of the discharge does not tell you whether it is normal. The discharge can look milky, clear, yellow, green, or brown.
Squeezing your nipple to check for discharge can make it worse. Leaving the nipple alone may make the discharge stop.
Exams and Tests
Your health care provider will examine you and ask questions about your symptoms and medical history.
Tests that may be done include:
- Prolactin blood test
- Thyroid blood tests
- Head CT scan or MRI to look for pituitary tumor
- Mammography
- Ultrasound of the breast
- Breast biopsy
- Ductography or ductogram: an x-ray with contrast dye injected into the affected milk duct
- Skin biopsy, if Paget disease is a concern
Treatment
Once the cause of your nipple discharge is found, your provider can recommend ways to treat it. You may:
- Need to change any medicine that caused the discharge
- Have lumps removed
- Have all or some of the breast ducts removed
- Receive creams to treat skin changes around your nipple
- Receive medicines to treat a health condition that is causing the nipple discharge
If all of your tests are normal, you may not need treatment. You should have another mammogram and physical exam within 1 year.
Outlook (Prognosis)
Most of the time, nipple problems are not breast cancer. These problems will either go away with the right treatment, or they can be watched closely over time.
Possible Complications
Nipple discharge may be a symptom of breast cancer or a pituitary tumor.
Skin changes around the nipple may be caused by Paget disease.
When to Contact a Medical Professional
Have your provider evaluate any nipple discharge.
Related Information
Intraductal papillomaEndocrine glands
Breast cancer
References
Klimberg VS, Hunt KK. Diseases of the breast. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 35.
Leitch AM, Ashfaq R. Discharges and secretions of the nipple. In: Klimberg VS, Gradishar WJ, Bland KI, Korourian S, White J, Copeland EM, eds. Bland and Copeland's The Breast: Comprehensive Management of Benign and Malignant Diseases. 6th ed. Philadelphia, PA: Elsevier; 2024:chap 6.
Sandadi S, Rock DT, Orr JW, Valela FA. Breast diseases: detection, management, and surveillance of breast disease. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 15.
Swartz MH, Nentin FG. The breast. In: Swartz MH, ed. Textbook of Physical Diagnosis: History and Examination. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 16.
BACK TO TOPReview Date: 10/17/2024
Reviewed By: Linda J. Vorvick, MD, Clinical Professor, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
