Health Library
Scar revision
Keloid revision; Hypertrophic scar revision; Scar repair; Z-plasty
Scar revision is surgery to improve or reduce the appearance of scars. It also restores function, and corrects skin changes (disfigurement) caused by an injury, wound, poor healing, or previous surgery.
Images



Presentation

I Would Like to Learn About:
Description
Scar tissue forms as skin heals after an injury (such as an accident) or surgery.
How much scarring there is depends on:
- Size, depth, and location of the wound
- Your age
- Skin characteristics, such as color (pigmentation)
Depending on the extent of the surgery, scar revision can be done while you are awake (local anesthesia), sleeping (sedated), or deep asleep and pain-free (general anesthesia).
When to have scar revision done is not always clear. Scars shrink and become less noticeable as they age. You may be able to wait to have surgery until the scar lightens in color. This can be several months or even a year after the wound has healed. For some scars, it is best to have revision surgery 60 to 90 days after the scar matures or longer. Each scar is different.
There are several ways to improve the appearance of scars:
- The scar may be removed completely and the new wound closed very carefully.
- Scar massage and pressure therapy, such as silicone strips.
- Dermabrasion involves removing the upper layers of the skin with a special wire brush called a burr or fraise. New skin grows over this area. Dermabrasion can be used to soften the surface of the skin or reduce irregularities.
- A laser may be used to soften the surface of the scar, and stimulate new collagen growth within the scar.
- Steroid injection may be given to soften or shrink the scar.
- Very large injuries (such as burns) can cause loss of a large area of skin and may form hypertrophic scars. These types of scars can restrict movement of muscles, joints and tendons (contracture). Surgery removes extra scar tissue. It may involve a series of small cuts (incisions) on both sides of the scar site, which create V-shaped skin flaps (Z-plasty). The result is a thin, less noticeable scar, because a Z-plasty may re-orient the scar so that it more closely follows the natural skin folds and releases tightness in the scar, but lengthens the scar during the process.
- Skin grafting involves taking a thin layer of skin from another part of the body and placing it over the injured area. Skin flap surgery involves moving an entire, full thickness of skin, fat, nerves, blood vessels, and muscle from a healthy part of the body to the injured site. These techniques are used when a large amount of skin has been lost in the original injury, when a thin scar will not heal, and when the main concern is improved function rather than improved appearance.
- Tissue expansion is used for breast reconstruction. It is also used for skin that has been damaged due to birth defects and injuries. A silicone balloon is inserted beneath the skin and gradually filled with salt water. This stretches the skin, which grows over time.
Why the Procedure Is Performed
Problems that may indicate a need for scar revision include:
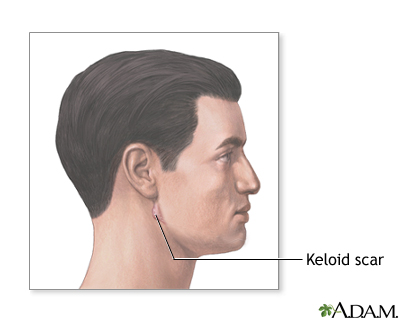
- A keloid, which is an abnormal scar that is thicker and of a different color and texture than the rest of the skin. Keloids extend beyond the edge of the wound and are likely to come back. They often create a thick, puckered effect that looks like a tumor. Keloids are removed at the place where they meet normal tissue.
- A scar that is at an angle to the normal tension lines of the skin.
- A scar that is thickened.
- A scar that causes distortion of other features or causes problems with normal movement or function.
Risks
Risks of anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, infection
Risks of scar revision surgery are:
- Scar recurrence
- Keloid formation (or recurrence)
- Separation or reopening (dehiscence) of the wound
Exposing the scar to too much sun may cause it to darken, which could interfere with future revision.
After the Procedure
For keloid revision, a pressure or elastic dressing may be placed over the area after the operation to prevent the keloid from coming back.
For other types of scar revision, a light dressing is applied. Stitches are usually removed after 3 to 4 days for the facial area, and after 5 to 7 days for incisions on other parts of the body.
When you return to normal activities and work depends on the type, degree, and location of the surgery. Most people can resume normal activities soon after surgery. Your health care provider will likely tell you to avoid activities that stretch and may widen the new scar.
If you have long-term stiffening of the joint, you may need physical therapy after surgery.
Apply sunscreen to keep sunlight from permanently tanning the healing scar.
Related Information
KeloidsContracture deformity
References
Hu MS, Zielins ER, Longaker MT, Lorenz HP. Scar prevention, treatment, and revision. In: Gurtner GC, Neligan PC, eds. Plastic Surgery, Volume 1: Principles. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 14.
Leitenberger JJ, Isenhath SN, Swanson NA, Lee KK. Scar revision. In: Robinson JK, Hanke CW, Siegel DM, Fratila A, Bhatia AC, Rohrer TE, eds. Surgery of the Skin: Procedural Dermatology. 3rd ed. Philadelphia, PA: Elsevier; 2015:chap 21.
McCrary HC, Mobley SR. Scar revision, keloids, and camouflage. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
BACK TO TOPReview Date: 5/26/2023
Reviewed By: Tang Ho, MD, Associate Professor, Division of Facial Plastic and Reconstructive Surgery, Department of Otolaryngology - Head and Neck Surgery, The University of Texas Medical School at Houston, Houston, TX. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
