Health Library
Apgar score
Newborn scoring; Delivery - Apgar
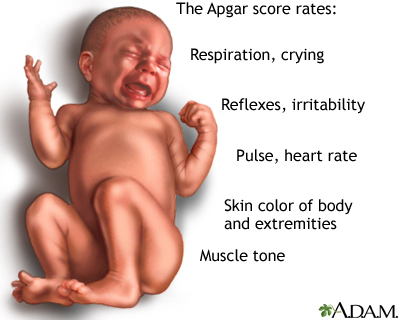
Apgar is a quick test performed on a baby at 1 and 5 minutes after birth. The 1-minute score determines how well the baby tolerated the birthing process. The 5-minute score tells the health care provider how well the baby is doing outside the mother's womb. It also helps measure how well the baby responds if resuscitation is needed right after birth.
In rare cases, the test will be done 10 minutes after birth.
Virginia Apgar, MD (1909-1974) introduced the Apgar score in 1952.
Images

I Would Like to Learn About:
How the Test is Performed
The Apgar test is done by a doctor, midwife, or nurse. The health care provider examines the baby's:
- Breathing effort
- Heart rate
- Muscle tone
- Reflexes
- Skin color
Each category is scored with 0, 1, or 2, depending on the observed condition.
Breathing effort:
- If the infant is not breathing, the respiratory score is 0.
- If the respirations are slow or irregular, the infant scores 1 for respiratory effort.
- If the infant cries well, the respiratory score is 2.
Heart rate is evaluated by stethoscope. This is the most important assessment:
- If there is no heartbeat, the infant scores 0 for heart rate.
- If heart rate is less than 100 beats per minute, the infant scores 1 for heart rate.
- If heart rate is greater than 100 beats per minute, the infant scores 2 for heart rate.
Muscle tone:
- If muscles are loose and floppy, the infant scores 0 for muscle tone.
- If there is some muscle tone, the infant scores 1.
- If there is active motion, the infant scores 2 for muscle tone.
Grimace response or reflex irritability is a term describing response to stimulation, such as a mild pinch:
- If there is no reaction, the infant scores 0 for reflex irritability.
- If there is grimacing, the infant scores 1 for reflex irritability.
- If there is grimacing and a cough, sneeze, or vigorous cry, the infant scores 2 for reflex irritability.
Skin color:
- If the skin color is pale blue, the infant scores 0 for color.
- If the body is pink and the extremities are blue, the infant scores 1 for color.
- If the entire body is pink, the infant scores 2 for color.
Why the Test is Performed
This test is done to determine whether a newborn needs help breathing or is having heart trouble.
Normal Results
The Apgar score is based on a total score of 1 to 10. The higher the score, the better the baby is doing after birth.
A score of 7, 8, or 9 is normal and is a sign that the newborn is in good health. A score of 10 is very unusual, since almost all newborns lose 1 point for blue hands and feet, which is normal for after birth.
What Abnormal Results Mean
Any score lower than 7 is a sign that the baby needs medical attention. The lower the score, the more help the baby needs to adjust outside the mother's womb.
Most of the time a low Apgar score is caused by:
- A difficult birth
- C-section
- Fluid in the baby's airway
A baby with a low Apgar score may need:
- Oxygen and clearing out the airway to help with breathing
- Physical stimulation to get the heart beating at a healthy rate
Most of the time, a low score at 1 minute is near-normal by 5 minutes. Apgar scores are not usually measured after 5 minutes.
A lower Apgar score does not mean a child will have serious or long-term health problems. The Apgar score is not designed to predict the future health of the child.
If the Apgar score is below 7 at the five-minute mark, some providers will check it a few minutes later to assess the effect of any action taken to correct any respiratory or cardiac concerns. If it is rechecked, that typically stops once the Apgar score has reached 7.
Related Information
Newborn screening testsReferences
Arulkumaran S. Fetal surveillance in labor. In: Arulkumaran SS, Robson MS, eds. Munro Kerr's Operative Obstetrics. 13th ed. Philadelphia, PA: Elsevier; 2020:chap 9.
Goyal NK. The newborn infant. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 113.
BACK TO TOPReview Date: 10/22/2022
Reviewed By: Charles I. Schwartz MD, FAAP, Clinical Assistant Professor of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, General Pediatrician at PennCare for Kids, Phoenixville, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
