Health Library
Bilirubin encephalopathy
Bilirubin-induced neurologic dysfunction (BIND); Kernicterus
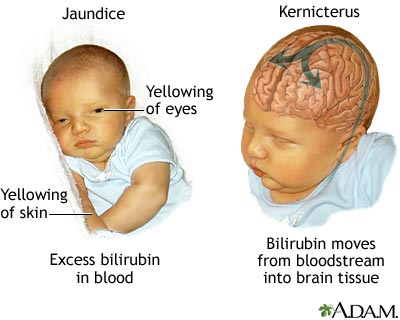
Bilirubin encephalopathy is a rare neurological condition that occurs in some newborns with severe jaundice.
Images
I Would Like to Learn About:
Causes
Bilirubin encephalopathy (BE) is caused by very high levels of bilirubin. Bilirubin is a yellow pigment that is created as the body gets rid of old red blood cells. High levels of bilirubin in the body can cause the skin to look yellow (jaundice).
If the level of bilirubin is very high or a baby is very ill, the substance will move out of the blood and collect in the brain tissue if it is not bound to albumin (protein) in the blood. This can lead to problems such as brain damage and hearing loss. The term "kernicterus" refers to the yellow staining caused by bilirubin. This is seen in parts of the brain on autopsy.
This condition most often develops in the first week of life, but may be seen up until the third week. Some newborns with Rh hemolytic disease are at high risk for severe jaundice that can lead to this condition. Rarely, BE can develop in seemingly healthy babies.
Symptoms
The symptoms depend on the stage of BE. Not all babies with kernicterus on autopsy have had definite symptoms.
Early stage:
- Extreme jaundice
- Absent startle reflex
- Poor feeding or sucking
- Extreme sleepiness (lethargy) and low muscle tone (hypotonia)
Middle stage:
- High-pitched cry
- Irritability
- May have arched back with neck hyperextended backwards, high muscle tone (hypertonia)
- Poor feeding
Late stage:
- Stupor or coma
- No feeding
- Shrill cry
- Muscle rigidity, markedly arched back with neck hyperextended backwards
- Seizures
Exams and Tests
A blood test will show a high bilirubin level (greater than 20 to 25 mg/dL). However, there is not a direct link between bilirubin level and degree of injury.
Normal value ranges may vary slightly among different laboratories. Talk to your health care provider about the meaning of your specific test results.
Treatment
Treatment depends on how old the baby is (in hours) and whether the baby has any risk factors (such as prematurity). It may include:
- Light therapy (phototherapy)
- Exchange transfusions (removing the child's blood and replacing it with fresh donor blood or plasma)
Outlook (Prognosis)
BE is a serious condition. Many infants with late-stage nervous system complications die.
Possible Complications
Complications may include:
- Permanent brain damage
- Hearing loss
- Death
When to Contact a Medical Professional
Get medical help right away if your baby has signs of this condition.
Prevention
Treating jaundice or conditions that may lead to it can help prevent this problem. Infants with the first signs of jaundice have bilirubin level measured within 24 hours. If the level is high, the infant should be screened for diseases that involve the destruction of red blood cells (hemolysis).
All newborns have a follow-up appointment within 2 to 3 days after leaving the hospital. This is very important for late preterm or early term babies (born more than 2 to 3 weeks before their due date).
Related Information
Newborn jaundice - dischargeReferences
Hamati AI, Felker MV. Neurological complications of systemic disease: children. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 59.
Hansen TWR. Pathophysiology of kernicterus. In: Polin RA, Abman SH, Rowitch, DH, Benitz WE, eds. Fetal and Neonatal Physiology. 6th ed. Philadelphia, PA: Elsevier; 2022:chap 163.
Kaplan M, Wong RJ, Burgis JC, Sibley E, Stevenson DK. Neonatal jaundice and liver disease. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 91.
Marcdante KJ, Kliegman RM, Schuh AM. Anemia and hyperbilirubinemia. In: Marcdante KJ, Kliegman RM, Schuh AM, eds. Nelson Essentials of Pediatrics. 9th ed. Elsevier; 2023:chap 62.
BACK TO TOPReview Date: 4/25/2023
Reviewed By: Charles I. Schwartz, MD, FAAP, Clinical Assistant Professor of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, General Pediatrician at PennCare for Kids, Phoenixville, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
