Skull fracture
Basilar skull fracture; Depressed skull fracture; Linear skull fracture
A skull fracture is a fracture or break in the skull (cranial) bones.
Considerations
Skull fractures may occur with head injuries. The skull provides good protection for the brain. However, a severe impact or blow can cause the skull to break. It may be accompanied by a concussion or other injury to the brain.
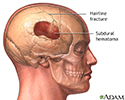
The brain can be affected directly by damage to the nervous system tissue and bleeding. The brain can also be affected by bleeding under the skull. This can compress the underlying brain tissue.
A simple fracture is a break in the bone without damage to the skin.
A linear skull fracture is a break in a cranial bone resembling a thin line, without splintering, depression, or distortion of bone.
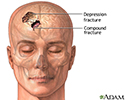
A depressed skull fracture is a break in a cranial bone (or "crushed" portion of skull) with depression of the bone in toward the brain.
A compound fracture involves a break in, or loss of, skin and splintering of the bone.
Causes
Causes of skull fracture can include:
- Head trauma
- Falls, automobile accidents, physical assault, and sports
Symptoms
Symptoms may include:
- Bleeding from wound, ears, nose, or around eyes
- Bruising behind the ears or under the eyes
- Changes in pupils (sizes unequal, not reactive to light)
- Confusion
- Convulsions (seizures)
- Difficulties with balance
- Drainage of clear or bloody fluid from ears or nose
- Drowsiness
- Headache
- Loss of consciousness (unresponsiveness)
- Nausea and vomiting
- Restlessness, irritability
- Slurred speech
- Stiff neck
- Swelling
- Visual disturbances
In some cases, the only symptom may be a bump on the head. A bump or bruise may take up to 24 hours to develop.
First Aid
Take the following steps if you think someone has a skull fracture:
- Check the airways, breathing, and circulation. If necessary, begin rescue breathing and CPR.
- Avoid moving the person (unless absolutely necessary) until medical help arrives. Have someone call 911 or the local emergency number for medical assistance.
- If the person must be moved, take care to stabilize the head and neck. Place your hands on both sides of the head and under the shoulders. Do not allow the head to bend forward or backward, or to twist or turn.
- Carefully check the site of injury, but do not probe in or around the site with a foreign object. It can be hard to know if the skull is fractured or depressed (dented in) at the site of injury.
- If there is bleeding, apply firm pressure with a clean cloth over a broad area to control blood loss, but do not apply pressure directly onto a suspected skull fracture.
- If blood soaks through, do not remove the original cloth. Instead, apply more cloths on top, and continue to apply pressure.
- If the person is vomiting, stabilize the head and neck, and carefully turn the victim to the side to prevent choking on vomit.
- If the person is conscious and experiencing any of the previously listed symptoms, transport to the nearest emergency medical facility (even if the person does not think medical help is needed).
Do Not
Follow these precautions:
- Do not move the person unless absolutely necessary. Head injuries may be associated with spinal injuries.
- Do not remove protruding objects.
- Do not allow the person to continue with physical activities.
- Do not forget to watch the person closely until medical help arrives.
- Do not give the person any medicines before talking to a health care provider.
- Do not leave the person alone, even if there are no obvious problems.
When to Contact a Medical Professional
The provider will perform a physical exam. The person's nervous system will be checked. There may be changes in the person's pupil size, thinking ability, coordination, and reflexes.
Get medical help right away if:
- There are problems with breathing or circulation.
- Direct pressure does not stop bleeding from the nose, ears, or wound.
- There is drainage of clear fluid from the nose or ears.
- There is facial swelling, bleeding, or bruising.
- There is an object protruding from the skull.
- The person is unconscious, is experiencing convulsions, has multiple injuries, appears to be in any distress, or cannot think clearly.
Tests that may be done include:
- Blood and urine tests
- Brain wave test [electroencephalogram (EEG)] may be needed if seizures are present
- Head CT scan
- MRI of the brain
- X-rays
Prevention
Not all head injuries can be prevented. The following simple steps can help keep you and your child safe:
- Always use safety equipment during activities that could cause a head injury. These include seat belts, bicycle or motorcycle helmets, and hard hats.
- Learn and follow bicycle safety recommendations.
- Do not drink and drive. Do not allow yourself to be driven by someone who may have been drinking alcohol or is otherwise impaired.
References
Bazarian JJ. Traumatic brain injury and spinal cord injury. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 368.
Papa L, Goldberg SA. Head trauma. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 33.
Roskind CG, Pryor HI, Klein BL. Acute care of multiple trauma. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA. Elsevier; 2020:chap 82.
Skull of an adult - illustration
Skull of an adult
illustration
Skull fracture - illustration
Skull fracture
illustration
Skull fracture - illustration
Skull fracture
illustration
Battle's sign - behind the ear - illustration
Battle's sign - behind the ear
illustration
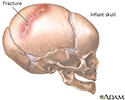
Infant skull fracture - illustration
Infant skull fracture
illustration
Review Date: 11/2/2023