Prerenal azotemia
Azotemia - prerenal; Uremia; Renal underperfusion; Acute renal failure - prerenal azotemia
Prerenal azotemia is an abnormally high level of nitrogen waste products in the blood.
Causes
Prerenal azotemia is common, especially in older adults and in people who are in the hospital.
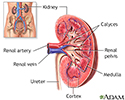
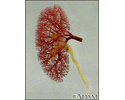
The kidneys filter the blood to make urine that removes waste products. When the amount, or pressure, of blood flow through the kidney drops, filtering of the blood also drops. Or it may not occur at all. Waste products stay in the blood. Less urine is made, even though the kidney itself is working.
When nitrogen waste products, such as creatinine and urea, build up in the body, the condition is called azotemia. These waste products act as poisons when they build up. They damage tissues and reduce the ability of the organs to function.
Prerenal azotemia is the most common form of reduced kidney function in hospitalized people. Any condition that reduces blood flow to the kidney may cause it, including:
- Burns
- Conditions that allow fluid to escape from the bloodstream
- Long-term vomiting, diarrhea, or bleeding
- Heat exposure
- Decreased fluid intake (dehydration)
- Loss of blood volume
- Certain medicines, such as ACE inhibitors (medicines that treat heart failure or high blood pressure) and non-steroidal anti-inflammatory drugs (NSAIDs)
Conditions in which the heart cannot pump enough blood or pumps blood at a low volume also increase the risk for prerenal azotemia. These conditions include:
- Heart failure
- Shock (septic shock)
It can also be caused by conditions that interrupt blood flow to the kidney, such as:
- Certain types of surgery
- Injury to the kidney
Symptoms
Prerenal azotemia may have no symptoms. Or, symptoms of the causes of prerenal azotemia may be present.
Symptoms of dehydration may be present and include any of the following:
- Confusion
- Decreased or no urine production
- Dry mouth due to thirst
- Fast pulse
- Fatigue
- Pale skin color
- Swelling
Exams and Tests
An exam may show:
- Collapsed neck veins
- Dry mucous membranes
- Little or no urine in the bladder
- Low blood pressure
- Low heart function or hypovolemia
- Poor skin elasticity (turgor)
- Rapid heart rate
- Reduced pulse pressure
- Signs of acute kidney failure
The following tests may be done:
- Blood creatinine
- Blood urea nitrogen (BUN)
- Urine osmolality and specific gravity
- Urine tests to check sodium and creatinine levels and to monitor kidney function
Treatment
The main goal of treatment is to quickly correct the cause before the kidney becomes damaged. People often need to stay in the hospital.
Intravenous (IV) fluids, including blood or blood products, may be used to increase blood volume. After blood volume has been restored, medicines may be used to:
- Increase blood pressure
- Improve the pumping of the heart
If the person has symptoms of acute kidney failure, treatment will likely include:
- Dialysis
- Diet changes
- Medicines
Outlook (Prognosis)
Prerenal azotemia can be reversed if the cause can be found and corrected within 24 hours. If the cause is not fixed quickly, damage may occur to the kidney (acute tubular necrosis).
Possible Complications
Complications may include:
- Acute kidney failure
- Acute tubular necrosis (tissue death)
When to Contact a Medical Professional
Go to the emergency room or call 911 or the local emergency number if you have symptoms of prerenal azotemia.
Prevention
Quickly treating any condition that reduces the volume or force of blood flow through the kidneys may help prevent prerenal azotemia.
References
Okusa MD, Portilla D. Pathophysiology of acute kidney injury. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 28.
Paine CH, Jefferson JA, Velez JCQ. Pathophysiology and etiology of acute kidney injury. In: Johnson RJ, Floege J, Tonelli M, eds. Comprehensive Clinical Nephrology. 7th ed. Philadelphia, PA: Elsevier; 2024:chap 70.
Wolfson AB. Renal failure. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 83
Review Date: 10/28/2024