Cranial mononeuropathy III
Third cranial nerve palsy; Oculomotor palsy; Pupil-involving third cranial nerve palsy; Mononeuropathy - compression type
Cranial mononeuropathy III is a nerve disorder. It affects the function of the third cranial nerve. As a result, the person may have double vision and eyelid drooping.
Causes
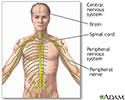
Mononeuropathy means that only one nerve is affected. This disorder affects the third cranial nerve in the skull. This is one of the cranial nerves that control eye movement. Causes may include:
- Brain aneurysm
- Infections
- Abnormal blood vessels (vascular malformations)
- Cavernous sinus thrombosis
- Tissue damage from loss of blood flow (infarction)
- Trauma (from head injury or caused accidentally during surgery)
- Tumors or other growths (especially tumors at the base of the brain and pituitary gland)
- Rarely, third nerve palsy can be present at birth (congenital)
- Increased brain pressure (brain herniation)
In rare cases, people with migraine headaches have a temporary problem with the oculomotor nerve. This is probably due to a spasm of the blood vessels. In some cases, no cause can be found.
People with diabetes may also develop a neuropathy of the third nerve.
Symptoms
Symptoms may include:
- Double vision, which is the most common symptom
- Drooping of one eyelid (ptosis)
- Enlarged pupil that does not get smaller when a light shines on it
- Headache or eye pain
Other symptoms may occur if the cause is a tumor or swelling of the brain. Decreasing alertness is serious, because it could be a sign of brain damage or impending death.
Exams and Tests
An eye examination may show:
- Enlarged (dilated) pupil of the affected eye
- Eye movement abnormalities
- Eyes that are not aligned
- Drooping eye lid
Your health care provider will do a complete examination to find out if other parts of the nervous system are affected. Depending on the suspected cause, you may need:
- Blood tests
- Tests to look at blood vessels to the brain (cerebral angiogram, CT angiogram, or MR angiogram)
- MRI or CT scan of the brain
- Spinal tap (lumbar puncture)
You may need to be referred to a doctor who specializes in vision problems related to the nervous system (neuro-ophthalmologist).
Treatment
Some people get better without treatment. Treating the cause (if it can be found) may relieve the symptoms.
Other treatments to relieve symptoms may include:
- Corticosteroid medicines to reduce swelling and relieve pressure on the nerve (when caused by a tumor or injury)
- Eye patch or glasses with prisms to reduce double vision
- Pain medicines
- Surgery to treat eyelid drooping or eyes that are not aligned
Outlook (Prognosis)
Some people will respond to treatment. In a few others, permanent eye drooping or loss of eye movement will occur.
Causes such as brain swelling due to a tumor or stroke, or a brain aneurysm may be life threatening.
When to Contact a Medical Professional
Contact your provider if you have double vision and it does not go away in a few minutes, especially if you also have eyelid drooping.
Prevention
Quickly treating disorders that could press on the nerve may reduce the risk of developing cranial mononeuropathy III.
References
Rucker JC, Seay MD. Cranial neuropathies. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 103.
Tamhankar MA. Eye movement disorders: third, fourth, and sixth nerve palsies and other causes of diplopia and ocular misalignment. In: Liu GT, Volpe NJ, Galetta SL, eds. Liu, Volpe, and Galetta's Neuro-Ophthalmology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 15.
Wallenstein J. Brain and cranial nerve disorders. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 91.
Review Date: 6/13/2024