Contact dermatitis
Dermatitis - contact; Allergic dermatitis; Dermatitis - allergic; Irritant contact dermatitis; Skin rash - contact dermatitis
Contact dermatitis is a condition in which the skin becomes red, sore, or inflamed after direct contact with a substance.
Causes
There are 2 types of contact dermatitis.
Irritant dermatitis: This is the most common type. It is not caused by an allergy, but rather the skin's reaction to irritating substances or friction. Irritating substances may include acids, alkaline materials such as soaps and detergents, fabric softeners, solvents, or other chemicals. Very irritating chemicals may cause a reaction after just a short period of contact. Milder chemicals can also cause a reaction after repeated contact.
People who have atopic dermatitis are at increased risk of developing irritant contact dermatitis.
Common materials that may irritate your skin include:
- Cement
- Hair dyes
- Long-term exposure to wet diapers
- Pesticides or weed killers
- Rubber gloves
- Shampoos
Allergic contact dermatitis: This form of the condition occurs when your skin comes in contact with a substance that causes you to have an allergic reaction.
Common allergens include:
- Adhesives, including those used for false eyelashes or toupees.
- Antibiotics, such as neomycin rubbed on the surface of the skin.
- Balsam of Peru (used in many personal products and cosmetics, as well as in many foods and drinks).
- Fabrics and clothing, including both materials and dyes.
- Fragrances in perfumes, cosmetics, soaps, and moisturizers.
- Nail polish, hair dyes, and permanent wave solutions.
- Nickel or other metals (found in jewelry, watch straps, metal zips, bra hooks, buttons, pocketknives, lipstick holders, and powder compacts).
- Poison ivy, poison oak, poison sumac, and other plants.
- Rubber or latex gloves or shoes.
- Preservatives commonly used in prescription and over-the-counter topical medicines.
- Formaldehyde, which is used in a broad number of manufactured items.
You will not have an allergic reaction to a substance when you are first exposed to the substance. However, you will form a reaction after future exposures. You may become more sensitive and develop a reaction if you use it regularly. It is possible to tolerate the substance for years or even decades before developing allergy. Once you develop an allergy you will be allergic for life.
The reaction most often occurs 24 to 48 hours after the exposure. The rash may persist for weeks after the exposure stops.
Some products cause a reaction only when the skin is also exposed to sunlight (photosensitivity). These include:
- Shaving lotions
- Sunscreens
- Sulfa ointments
- Some perfumes
- Coal tar products
- Oil from the skin of a lime
A few airborne allergens, such as ragweed, perfumes, vapor from nail lacquer, or insecticide spray, can also cause contact dermatitis.
Symptoms
Symptoms vary, depending on the cause and whether the dermatitis is due to an allergic reaction or an irritant. The same person may also have different symptoms over time.
Allergic reactions may occur suddenly, or develop after months or years of exposure.
Contact dermatitis often occurs on the hands. Hair products, cosmetics, and perfumes can lead to skin reactions on the face, head, and neck. Jewelry can also cause skin problems in the area under it.
Itching is a common symptom. In the case of an allergic dermatitis, itching can be severe.
You may have red, streaky, or patchy rash where the substance touched the skin. The allergic reaction is often delayed so that the rash may not appear until 24 to 48 hours after exposure.
The rash may:
- Have red bumps that may form moist, weeping blisters
- Feel warm and tender
- Ooze, drain, or crust
- Become scaly, raw, or thickened
Dermatitis caused by an irritant may also cause burning or pain as well as itching. Irritant dermatitis often shows as dry, red, and rough skin. Cuts (fissures) may form on the hands. Skin may become inflamed with long-term exposure.
Exams and Tests
Your health care provider will make the diagnosis based on how the skin looks and by asking questions about substances you may have come in contact with.
Allergy testing with skin patches (called patch testing) may be necessary to determine what is causing the reaction. Patch testing is used for certain people who have long-term or repeated contact dermatitis. It requires at least 3 office visits and must be done by a provider with the skill to interpret the results correctly.
- On the first visit, small patches of possible allergens are applied to the skin. These patches are removed at the second visit 48 hours later to see if a reaction has occurred.
- A third visit, about 2 days later, is done to look for any delayed reaction. For certain allergens such as metals, a final visit may be necessary on the 10th day.
- If you have already tested a material on a small area of your skin and noticed a reaction, you should bring the material with you.
Other tests may be used to rule out other possible causes, including skin lesion biopsy or culture of the skin lesion.
Treatment
Your provider will recommend treatment based on what is causing the problem. In some cases, the best treatment is to do nothing to the area.
Often, treatment includes washing the area with a lot of water to get rid of any traces of the irritant that are still on the skin. You should avoid further exposure to the substance.
Emollients or moisturizers help keep the skin moist, and also help skin repair itself. They protect the skin from becoming inflamed again. They are a key part of preventing and treating irritant contact dermatitis.
Topical corticosteroid medicines are commonly used to treat contact dermatitis.
- Topical means you place it on the skin. You will be prescribed a cream or ointment. Topical corticosteroids may also be called topical steroids or topical cortisones.
- DO NOT use more medicine or use it more often than your provider advises you to use it.
Your provider may also prescribe other creams or ointments, such as tacrolimus or pimecrolimus, to use on the skin.
In severe cases, you may need to take corticosteroid pills. Your provider will start you on a high dose and your dose will be slowly reduced over about 12 days. You may also receive a corticosteroid shot.
Wet dressings and soothing anti-itch (antipruritic) lotions may be recommended to reduce other symptoms.
Topical corticosteroids should be used only for short periods. Long-term use increases the risk of developing more irritant contact dermatitis.
Outlook (Prognosis)
Contact dermatitis clears up without complications in 2 or 3 weeks in most cases. However, it may return if the substance that caused it cannot be determined and avoided.
You may need to change your job or job habits if the disorder is caused by exposure at work. For example, jobs requiring frequent hand washing may be bad choices for people with hand dermatitis.
Sometimes, the allergen causing the allergic contact dermatitis reaction is never identified.
Possible Complications
Bacterial skin infections may occur.
When to Contact a Medical Professional
Contact your provider if:
- You have symptoms of contact dermatitis.
- The skin reaction is severe.
- You do not get better after treatment.
- Signs of infection such as tenderness, redness, warmth, or fever.
References
Dinulos JGH. Contact dermatitis and patch testing. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 4.
James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM. Contact dermatitis and drug eruptions. In: James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM, eds. Andrews' Diseases of the Skin: Clinical Dermatology. 13th ed. Philadelphia, PA: Elsevier; 2020:chap 6.
Nixon RL, Allnutt KJ, Diepgen TL. Contact dermatitis. In: Burks AW, Holgate ST, O'Hehir RE, et al, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 34.
Nixon RL, Mowad CM, Marks JG. Allergic contact dermatitis. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 14.
Poison oak rash on the arm - illustration
Poison oak rash on the arm
illustration
Latex allergy - illustration
Latex allergy
illustration
Poison plants - illustration
Poison plants
illustration
Dermatitis, nickel on the sole - illustration
Dermatitis, nickel on the sole
illustration
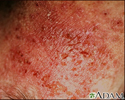
Dermatitis - contact - illustration
Dermatitis - contact
illustration
Dermatitis de contacto alérgica - vista de cerca - illustration
Dermatitis de contacto alérgica - vista de cerca
illustration
Dermatitis - contact on the cheek - illustration
Dermatitis - contact on the cheek
illustration
Dermatitis - pustular contact - illustration
Dermatitis - pustular contact
illustration
Poison ivy on the knee - illustration
Poison ivy on the knee
illustration
Poison ivy on the leg - illustration
Poison ivy on the leg
illustration
Photocontact dermatitis on the hand - illustration
Photocontact dermatitis on the hand
illustration
Review Date: 7/1/2023