Kawasaki disease
Mucocutaneous lymph node syndrome; Infantile polyarteritis; Kawasaki syndrome
Kawasaki disease is a rare condition that involves inflammation of the blood vessels. It occurs in children.
Causes
Kawasaki disease occurs most often in Japan, where it was first discovered. The disease is seen more often in boys than in girls. Most of the children who develop this condition are younger than age 5.
Kawasaki disease is not well understood and the cause is yet unknown. It may be an autoimmune disorder. The problem affects the mucous membranes, lymph nodes, walls of the blood vessels, and the heart.
Symptoms
Kawasaki disease often begins with a fever of 102°F (38.9°C) or higher that does not go away. The fever is often as high as 104°F (40°C). A fever lasting at least 5 days is a common sign of the disorder. The fever may last for up to 2 weeks. The fever often does not come down with normal doses of acetaminophen (Tylenol) or ibuprofen.
Other symptoms often include:
- Bloodshot or red eyes (without pus or drainage)
- Bright red, chapped, or cracked lips
- Red mucous membranes in the mouth
- "Strawberry" tongue, with white coating on the tongue, or visible red bumps on the back of the tongue
- Red, swollen palms of the hands and the soles of the feet
- Skin rashes on the middle of the body, not blister-like
- Peeling skin in the genital area, hands, and feet (mostly around the nails, palms, and soles)
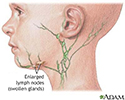
- Swollen lymph nodes in the neck (often only one lymph node is swollen)
- Joint pain and swelling, often on both sides of the body
Additional symptoms may include:
- Irritability
- Diarrhea, vomiting, and abdominal pain
- Cough and runny nose
Exams and Tests
Tests alone cannot diagnose Kawasaki disease. Most of the time, the health care provider will diagnose the disease when a child has most of the common symptoms.
In some cases, a child may have a fever that lasts more than 5 days, but not all the common symptoms of the disease. These children may be diagnosed with atypical Kawasaki disease.
All children with fever lasting more than 5 days should be checked for Kawasaki disease by a provider. Children with the disease need early treatment for a good outcome.
The following tests may be done:
- Chest x-ray
- Complete blood count
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Ferritin
- Serum albumin
- Serum transaminase
- Urinalysis - may show pus in the urine or protein in the urine
- Throat culture for streptococcus
- Echocardiogram
- Electrocardiogram
Tests such as ECG and echocardiography are done to look for signs of myocarditis, pericarditis, and inflammation of the coronary arteries. Arthritis and aseptic meningitis can also occur.
Treatment
Children with Kawasaki disease need hospital treatment. Treatment must be started right away to prevent damage to the coronary arteries and heart.
Intravenous gamma globulin is the standard treatment. It is given in high doses as a single infusion. The child's condition often gets much better within 24 hours of treatment with IV gamma globulin.
High-dose aspirin is often given along with IV gamma globulin.
Even with standard treatment, up to 1 in 4 children may still develop problems in their coronary arteries. In sicker children or those with signs of heart disease, adding corticosteroids is recommended. Tumor necrosis factor (TNF) inhibitors such as infliximab (Remicade) or etanercept (Enbrel) are not recommended for initial treatment. However, there still needs to be better tests to tell which children will benefit from these medicines.
Outlook (Prognosis)
Most children can recover fully when the disease is caught and treated early. About 1 in 100 children die from heart problems caused by the disease. People who have had Kawasaki disease should have an echocardiogram every 1 to 2 years to check for heart problems.
Possible Complications
Kawasaki disease can cause inflammation of blood vessels in the arteries, especially the coronary arteries. This can lead to aneurysm. Rarely, it can lead to a heart attack at a young age or later in life.
When to Contact a Medical Professional
Call your provider if symptoms of Kawasaki disease develop. Cracked, red lips and swelling and redness develop in the affected areas such as the palms and soles of the feet. If these problems occur along with an ongoing high fever that does not come down with acetaminophen or ibuprofen, your child should be checked by a provider.
Prevention
There are no known ways to prevent this disorder.
References
Abrams JY, Belay ED, Uehara R, Maddox RA, Schonberger LB, Nakamura Y. Cardiac complications, earlier treatment, and initial disease severity in Kawasaki disease. J Pediatr. 2017;188:64-69. PMID: 28619520 pubmed.ncbi.nlm.nih.gov/28619520/.
American Academy of Pediatrics. Kawasaki disease. In: Committee on Infectious Diseases, American Academy of; Pediatrics, Kimberlin DW, Barnett ED, Lynfield R, Sawyer MH, eds. Red Book: 2021-2024 Report of the Committee on Infectious Diseases. 32nd ed. Itasca, IL: American Academy of Pediatrics; 2021.
McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927-e999. PMID: 28356445 pubmed.ncbi.nlm.nih.gov/28356445/.
Nyhan A. Cardiology. In: Kleinman K, Mcdaniel L, Molloy M, eds. Harriet Lane Handbook, The. 22nd ed. Philadelphia, PA: Elsevier; 2021:chap 7.
Xue LJ, Wu R, Du GL, et al. Effect and safety of TNF inhibitors in immunoglobulin-resistant Kawasaki Disease: a meta-analysis. Clin Rev Allergy Immunol. 2017;52(3):389-400. PMID: 27550227 pubmed.ncbi.nlm.nih.gov/27550227/.
Review Date: 4/30/2023