Appendectomy
Appendix removal; Surgery - appendectomy; Appendicitis - appendectomy
An appendectomy is surgery to remove the appendix.

Description
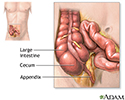
The appendix is a small, finger-shaped organ that branches off from the first part of the large intestine (colon). When it becomes swollen (inflamed) or infected, the condition is called appendicitis. When you have appendicitis, your appendix may need to be removed. An appendix that has a hole in it can leak and infect the entire abdomen area. This can be life threatening.
Appendectomy is done using either:
- Spinal anesthesia -- Medicine is put into your lower back to make you numb below your waist. You will also get medicine to make you sleepy.
- General anesthesia -- You will be asleep and not feel any pain during the surgery.
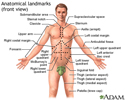
Your surgeon may make a small cut in the lower right side of your belly area and remove the appendix.
Your appendix can also be removed using small surgical cuts and a camera. This is called a laparoscopic appendectomy.
If your appendix broke open or a pocket of infection (abscess) formed, your abdomen may be washed out during surgery. A small tube may be left in the belly area to help drain out fluids or pus.

Why the Procedure Is Performed
An appendectomy is done for appendicitis. The condition can be hard to diagnose, especially in children, older people, and women of childbearing age.
Most often, the first symptom is pain around your belly button:
- The pain may be mild at first, but it becomes sharp and severe.
- The pain often moves into your right lower abdomen and becomes more focused in this area.
Other symptoms include:
- Diarrhea or constipation
- Fever (usually not very high)
- Nausea and vomiting
- Reduced appetite
If you have symptoms of appendicitis, seek medical help right away. Do not use heating pads, enemas, laxatives, or other home treatments to try to relieve symptoms.
Your health care provider will examine your abdomen and may perform a rectal exam and pelvic exam. Other tests may be done:
- Blood tests, including a white blood cell (WBC) count, may be done to check for infection.
- Your provider may order a CT scan or ultrasound to determine if the appendix is the cause of the problem since other illnesses can cause the same or similar symptoms.
The goal is to remove an infected appendix before it breaks open (ruptures). After reviewing your symptoms and the results of the physical exam and medical tests, your surgeon will decide whether you need surgery.
Risks
Risks of anesthesia and surgery in general include:
- Reactions to medicines
- Problems breathing
- Bleeding, blood clots, or infection
Risks of an appendectomy after a ruptured appendix include:
- Buildup of pus (abscess), which may need draining and antibiotics
- Infection of the incision
After the Procedure
Most people leave the hospital in 1 to 2 days after surgery. You can go back to your normal activities within a few weeks after leaving the hospital though it may take several weeks to get back to your normal energy level.
If you had laparoscopic surgery, you will likely recover quickly. Recovery is slower and more complicated if your appendix has broken open or an abscess has formed.
Living without an appendix causes no known health problems.
References
Quick CRG, Biers SM, Arulampalam THA. Appendicitis. In: Quick CRG, Biers SM, Arulampalam THA, eds. Essential Surgery: Problems Diagnosis and Management. 6th ed. Philadelphia, PA: Elsevier Limited; 2020:chap 26.
Richmond B. The appendix. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 51.
Rosenthal MD, Sarosi GS. Appendicitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 120.
Review Date: 3/31/2024