Breast reduction
Reduction mammoplasty; Macromastia - reduction
Breast reduction is surgery to reduce the size of the breasts.
Description
Breast reduction surgery is done under general anesthesia. This is medicine that keeps you asleep and pain-free.
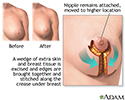
For a breast reduction, the surgeon removes some of the breast tissue and skin. Your nipples may be moved higher to reposition them for cosmetic reasons.
In the most common procedure:
- The surgeon makes three surgical cuts (incisions) around the areola (the dark area around your nipples), from the areola down to the crease under your breast, and across the lower crease of your breast.
- Extra fat, skin, and breast tissue are removed. The nipple and areola are moved to a higher position. Often the areola is made smaller.
- The surgeon closes the cuts with stitches to reshape the breast.
- Sometimes liposuction is combined with breast reduction to improve the shape of the breast and armpit areas.
The procedure can last 2 to 5 hours.
Why the Procedure Is Performed
Breast reduction may be recommended if you have very large breasts (macromastia) and:
- Chronic pain that affects your quality of life. You may be having headaches, neck pain, or shoulder pain.
- Chronic nerve problems caused by poor posture, which result in numbness or tingling in your arms or hands.
- Cosmetic problems, such as persistent bra-strap groove, scar-like lines in the skin (striae), difficulty finding clothes that fit, and low self-confidence.
- Chronic rashes under your breasts.
- Unwelcome attention that is making you feel awkward.
- Inability to participate in sports.
Some women may benefit from non-surgical treatments, such as:
- Exercising to strengthen their back and shoulder muscles
- Losing excess weight
- Wearing supportive bras
Risks
Risks of anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, or infection
Risks of this procedure are:
- Difficulty breastfeeding, or being unable to breastfeed
- Large scars that take a long time to heal
- Loss of feeling in the nipple area
- Uneven position of the nipples or differences in the size of the breasts
Before the Procedure
Ask your surgeon if you need a screening mammogram based on your age and risk of having breast cancer. This should be done long enough before surgery so if more imaging or a biopsy is needed, your planned surgery date won't be delayed.
Tell your surgeon or nurse:
- If you are or could be pregnant
- What medicines you are taking, even medicines, supplements, or herbs you bought without a prescription
The week or two before surgery:
- You may be asked to stop taking blood thinning medicines. These include aspirin, ibuprofen (Advil, Mortin), warfarin (Coumadin, Jantoven), and others.
- Ask your surgeon which medicines you should still take on the day of the surgery.
- If you smoke, try to stop. Smoking slows healing and increases the risk for problems. Ask your health care provider for help quitting.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Wear or bring loose clothing that buttons or zips in front.
- Arrive at the hospital on time.
After the Procedure
You may go home the same day or stay overnight in the hospital.
A gauze dressing (bandage) will be wrapped around your breasts and chest. Or, you will wear a surgical bra. Wear the surgical bra or a soft supportive bra for as long as your surgeon tells you to. This will likely be for several weeks.
Drainage tubes may be attached to your breasts. These tubes will be removed within a few days.
Your pain should decrease in a few weeks. Ask your surgeon if you can take acetaminophen (Tylenol) or ibuprofen (Advil) to help with pain instead of a narcotic medicine. If you do use a narcotic medicine, be sure to take it with food and plenty of water. Do not apply ice or heat to your breasts unless your surgeon has told you that is OK.
Ask your surgeon when it is OK to shower or bathe.
Within a few weeks, the swelling and bruising around your incisions should disappear. You may have a temporary loss of sensation in your breast skin and nipples after surgery. Sensation may return over time.
Follow any other self-care instructions you are given.
Schedule a follow-up visit with your surgeon. At that time you will be checked for how you are healing. Sutures (stitches) will be removed if needed.
Outlook (Prognosis)
You are likely to have a very good outcome from breast reduction surgery. You may feel better about your appearance and be more comfortable with various activities.
Pain or skin symptoms, such as striation, may disappear. You may need to wear a special supportive bra for a few months for comfort and to help with healing.
Scars are permanent. They will be more visible for the first year, but will then fade. The surgeon will make every effort to place the surgical cuts so that scars are hidden. Cuts are usually made on the underside of the breast and around the areola. Most of the time, the scars should not be noticeable, even in low-cut clothing.
References
American Board of Cosmetic Surgery website. Breast reduction guide. www.americanboardcosmeticsurgery.org/procedure-learning-center/breast/breast-reduction-guide/ www.americanboardcosmeticsurgery.org/procedure-learning-center/breast/breast-reduction-guide/. Accessed April 5, 2023.
Lista F, Austin RE, Ahmad J. Reduction mammaplasty with short scar techniques. In: Nahabedian MY, Neligan PC, eds. Plastic Surgery: Volume 5: Breast. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 10.
Review Date: 3/11/2023