Pediatric sleep apnea
Sleep apnea - pediatric; Apnea - pediatric sleep apnea syndrome; Sleep-disordered breathing - pediatric
With pediatric sleep apnea, a child's breathing pauses during sleep because the airway has become narrowed or partly blocked.
Causes
During sleep, all of the muscles in the body become more relaxed. This includes the muscles that help keep the throat open so air can flow into the lungs.
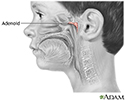
Normally, the throat remains open enough during sleep to let air pass by. However, some children have a narrow throat. This is often because of large tonsils or adenoids, which partially block the airflow. When the muscles in their upper throat relax during sleep, the tissues close in and block the airway. This stop in breathing is called apnea.
Other factors that also may increase the risk of sleep apnea in children include:
- A small jaw
- Certain shapes of the roof of the mouth (palate)
- Large tongue, which may fall back and block the airway
- Obesity
- Poor muscle tone due to conditions such as Down syndrome or cerebral palsy
Symptoms
Loud snoring is a telltale symptom of sleep apnea. Snoring is caused by air squeezing through the narrowed or blocked airway. However, not every child who snores has sleep apnea.
Children with sleep apnea also have the following symptoms at night:
- Long silent pauses in breathing followed by snorts, choking, and gasps for air
- Breathing mainly though the mouth
- Restless sleep
- Waking up often
- Sleepwalking
- Sweating
- Bedwetting
During the daytime, children with sleep apnea may:
- Feel sleepy or drowsy throughout the day
- Act grumpy, impatient, or irritable
- Have trouble concentrating in school
- Have hyperactive behavior
Exams and Tests
Your health care provider will take your child's medical history and do a physical exam.
- Your provider will check your child's mouth, neck, and throat.
- Your child may be asked about daytime sleepiness, how well they sleep, and bedtime habits.
Your child may be given a sleep study to confirm sleep apnea.
Treatment
Surgery to remove the tonsils and adenoids often cures the condition in children.
If needed, surgery also may be used to:
- Remove extra tissue at the back of the throat
- Correct problems with the structures in the face
- Create an opening in the windpipe to bypass the blocked airway if there are physical problems
Sometimes, surgery is not recommended or does not help. In that case, your child may use a continuous positive airway pressure (CPAP) device.
- Your child wears a mask over their nose during sleep.
- The mask is connected by a hose to a small machine that sits at the side of the bed.
- The machine pumps air under pressure through the hose and mask and into the airway during sleep. This helps keep the airway open.
It can take some time to get used to sleeping using CPAP therapy. Good follow-up and support from a sleep center can help your child overcome any problems using CPAP.
Other treatments may include:
- Inhaled nasal steroids.
- Dental device. This is inserted into the mouth during sleep to keep the jaw forward and the airway open.
- Weight loss, for overweight children.
Outlook (Prognosis)
In most cases, treatment completely relieves symptoms and problems from sleep apnea.
Possible Complications
Untreated pediatric sleep apnea may lead to:
- High blood pressure
- Heart or lung problems
- Slow growth and development
When to Contact a Medical Professional
Contact your provider if:
- You notice symptoms of sleep apnea in your child
- Symptoms don't improve with treatment, or new symptoms develop
References
Harsanyi K, Ratarasarn K, Amara AW, Maddox MH. Epidemiology of sleep medicine. In: Kryger M, Roth T, Goldstein CA, Dement WC, eds. Principles and Practice of Sleep Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 70.
Ishman SL, Prosser JD. Evaluation and management of persistent pediatric obstructive sleep apnea. In: Friedman M, Jacobowitz O, eds. Sleep Apnea and Snoring. 2nd ed. Philadelphia, PA: Elsevier; 2020:chap 69.
Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714-e755. PMID: 22926176 pubmed.ncbi.nlm.nih.gov/22926176.
Review Date: 7/1/2023