Health Library
Lung needle biopsy
Transthoracic needle aspiration; Percutaneous needle aspiration
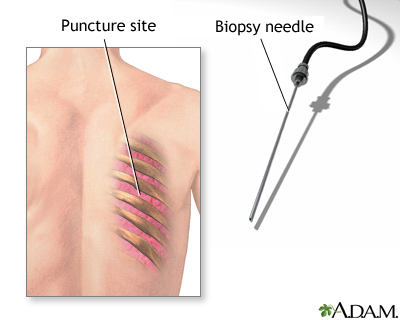
A lung needle biopsy is a method to remove a piece of lung tissue for examination. If it is done through the wall of your chest, it is called a transthoracic lung biopsy.
Images

I Would Like to Learn About:
How the Test is Performed
The procedure usually takes 30 to 60 minutes. The biopsy is done in the following way:
- A chest x-ray or chest CT scan may be used to find the exact spot for the biopsy. If the biopsy is done using a CT scan, you may be lying down during the exam.
- You may be given a sedative to relax you.
- You sit with your arms resting forward on a table. Your skin where the biopsy needle is inserted is scrubbed.
- A local painkilling medicine (anesthetic) is injected.
- Your surgeon makes a small cut in your skin.
- The biopsy needle is inserted into the abnormal tissue, tumor, or lung tissue. A small piece of tissue is removed with the needle.
- The needle is removed. Pressure is placed on the site. Once bleeding has stopped, a bandage is applied.
- A chest x-ray is taken right after the biopsy.
- The biopsy sample is sent to the lab. Analysis usually takes a few days.
How to Prepare for the Test
You should not eat for 6 to 12 hours before the test. Follow instructions about not taking nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, or blood thinners such as warfarin for a period of time before the procedure. Check with your health care provider before changing or stopping any medicines.
Before a needle biopsy of the lung, a chest x-ray or chest CT scan may be performed.
How the Test will Feel
You will receive an injection of anesthetic before the biopsy. This injection will sting for a moment. You will feel pressure and a brief, sharp pain when the biopsy needle touches the lung.
Why the Test is Performed
A lung needle biopsy is done when there is an abnormal condition near the surface of the lung, in the lung itself, or on the chest wall. Most often, it is done to check for cancer. The biopsy is usually done after abnormalities appear on a chest x-ray or CT scan. Sometimes your provider might recommend a bronchoscopy instead of lung needle biopsy depending on the location of the abnormality.
Normal Results
In a normal test, the tissues are normal and there is no cancer or growth of bacteria, viruses, or fungi if a culture is performed.
What Abnormal Results Mean
An abnormal result may be due to any of the following:
- Bacterial, viral, or fungal lung infection
- Cancerous cells (lung cancer, mesothelioma)
- Pneumonia
- Benign growth
Risks
Sometimes, a collapsed lung (pneumothorax) occurs after this test. A chest x-ray will be done after the biopsy to check for this. The risk is higher if you have certain lung diseases such as emphysema. Usually, a collapsed lung after a biopsy does not need treatment. But if the pneumothorax is large, there is preexisting lung disease or it does not improve, a chest tube is inserted to expand your lung.
In rare cases, pneumothorax can be life threatening if air escapes from the lung, gets trapped in the chest, and presses on the rest of your lungs or heart.
Whenever a biopsy is done, there is a risk of too much bleeding (hemorrhage). Some bleeding is common, and a provider will monitor the amount of bleeding. In rare cases, major and life-threatening bleeding can occur.
A needle biopsy should not be performed if other tests show that you have:
- A bleeding disorder of any type
- Bullae (enlarged alveoli that occur with emphysema)
- Cor pulmonale (condition that causes the right side of the heart to fail)
- Cysts of the lung
- High blood pressure in the lung arteries (pulmonary hypertension)
- Severe hypoxia (low oxygen)
Considerations
Signs of a collapsed lung include:
- Blueness of the skin
- Chest pain
- Rapid heart rate (rapid pulse)
- Shortness of breath
If any of these occur, call your provider right away.
Related Information
Community-acquired pneumonia in adultsLung cancer - small cell
Lung metastases
Aspiration pneumonia
References
Given MF, Clements W, Thomson KR, Lyon SM. Percutaneous biopsy and drainage of the lung, mediastinum, and pleura. In: Mauro MA, Murphy KPJ, Thomson KR, Venbrux AC, Morgan RA, eds. Image-Guided Interventions. 3rd ed. Philadelphia, PA: Elsevier; 2021:chap 103.
Walsh R, Klein JS. Thoracic radiology: invasive diagnostic imaging and image-guided interventions. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 21.
BACK TO TOPReview Date: 8/19/2024
Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
