Membranoproliferative glomerulonephritis
Membranoproliferative GN I; Membranoproliferative GN II; Mesangiocapillary glomerulonephritis; Membranoproliferative glomerulonephritis; Lobular GN; Glomerulonephritis - membranoproliferative; MPGN type I; MPGN type II
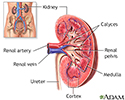
Membranoproliferative glomerulonephritis is a kidney disorder that involves inflammation and changes to kidney cells. It may lead to kidney failure.
Causes
Glomerulonephritis is an inflammation of the glomeruli. The glomeruli of the kidney help filter wastes and fluids from the blood to form urine.
Membranoproliferative glomerulonephritis (MPGN) is a form of glomerulonephritis caused by an abnormal immune response. Deposits of antibodies build up in a part of the kidneys called the glomerular basement membrane. This membrane helps filter wastes and extra fluids from the blood.
Damage to this membrane affects the kidney's ability to create urine normally. It may allow blood and protein to leak into the urine. If enough protein leaks into the urine, fluid may leak out of the blood vessels into body tissues, leading to swelling (edema). Nitrogen waste products may also build up in the blood (azotemia).
The 2 forms of this disease are MPGN I and MPGN II.
Most people with the disease have type I. MPGN II is much less common. It also tends to get worse faster than MPGN I.
Causes of MPGN may include:
- Autoimmune diseases (systemic lupus erythematosus, scleroderma, Sjögren syndrome, sarcoidosis)
- Cancer (leukemia, lymphoma)
- Infections (hepatitis B, hepatitis C, endocarditis, malaria)
Symptoms
Symptoms may include any of the following:
- Blood in the urine
- Changes in mental status such as decreased alertness or decreased concentration
- Cloudy urine
- Dark urine (smoke, cola, or tea colored)
- Decrease in urine volume
- Swelling of any part of the body
Exams and Tests
The health care provider will examine you and ask about your symptoms. The provider may find that you have signs of too much fluid in the body, such as:
- Swelling, often in the legs
- Abnormal sounds when listening to your heart and lungs with a stethoscope
- You may have high blood pressure
The following tests help confirm the diagnosis:
- BUN and creatinine blood test
- Blood complement levels
- Urinalysis
- Urine protein
- Kidney biopsy (to confirm membranoproliferative GN I or II)
Treatment
Treatment depends on the symptoms. The goals of treatment are to reduce symptoms, prevent complications, and slow the progression of the disorder.
You may need a change in diet. This may include limiting sodium, fluids, or protein to help control high blood pressure, swelling, and the buildup of waste products in the blood.
Medicines that may be prescribed include:
- Blood pressure medicines
- Dipyridamole, with or without aspirin
- Diuretics
- Medicines to suppress the immune system, such as cyclophosphamide
- Steroids
Treatment is more effective in children than in adults. Dialysis or kidney transplant may eventually be needed to manage kidney failure.
Outlook (Prognosis)
The disorder often slowly gets worse and eventually results in chronic kidney failure.
Half of people with this condition develop long-term (chronic) kidney failure within 10 years. This is more likely in those who have higher levels of protein in their urine.
Possible Complications
Complications that may result from this disease include:
When to Contact a Medical Professional
Contact your provider if:
- You have symptoms of this condition
- Your symptoms get worse or do not go away
- You develop new symptoms, including decreased urine output
Prevention
Preventing infections such as hepatitis or managing diseases such as lupus may help prevent MPGN.
References
Radhakrishnan J, Stokes MB. Glomerular disorders and nephrotic syndromes. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 107.
Saha MK, Pendergraft WF, Jennette JC, Falk RJ. Primary glomerular disease. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 31.
Sethi S, De Vriese AS, Fervenza FC. Immunoglobulin-mediated glomerulonephritis with a membranoproliferative pattern of injury and cryoglobulinemic glomerulonephritis. In: Johnson RJ, Floege J, Tonelli M, eds. Comprehensive Clinical Nephrology. 7th ed. Philadelphia, PA: Elsevier; 2024:chap 22.
Review Date: 8/28/2023
Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.