Proximal renal tubular acidosis
Renal tubular acidosis - proximal; Type II RTA; RTA - proximal; Renal tubular acidosis type II
Proximal renal tubular acidosis is a disease that occurs when the kidneys don't properly remove acids from the blood into the urine. As a result, too much acid remains in the blood (called acidosis).
Causes
When the body performs its normal functions, it produces acid. If this acid is not removed or neutralized, the blood will become too acidic. This can lead to electrolyte imbalances in the blood. It can also cause problems with normal function of some cells.
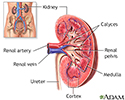
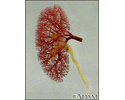
The kidneys help control the body's acid level by removing acid from the blood and excreting it into the urine. Acidic substances in the body are neutralized by alkaline substances, mainly bicarbonate.
Proximal renal tubular acidosis (type II RTA) occurs when bicarbonate is not properly reabsorbed by the kidney's filtering system.
Type II RTA is less common than type I RTA. Type I is also called distal renal tubular acidosis. Type II most often occurs during infancy and may go away by itself.
Causes of type II RTA include:
- Cystinosis (body is unable to break down the substance cysteine)
- Drugs such as ifosfamide (a chemotherapy drug), certain antibiotics that are no longer used much (tetracycline), or acetazolamide
- Fanconi syndrome, a disorder of the kidney tubes in which certain substances normally absorbed into the bloodstream by the kidneys are released into the urine instead
- Inherited fructose intolerance, a disorder in which there is a lack of the protein needed to break down the fruit sugar fructose
- Multiple myeloma, a type of blood cancer
- Primary hyperparathyroidism, a disorder in which the parathyroid glands in the neck produce too much parathyroid hormone
- Sjögren syndrome, an autoimmune disorder in which the glands that produce tears and saliva are destroyed
- Wilson disease, an inherited disorder in which there is too much copper in the body's tissues
- Vitamin D deficiency
Symptoms
Symptoms of proximal renal tubular acidosis include any of the following:
- Confusion or decreased alertness
- Dehydration
- Fatigue
- Increased breathing rate
- Osteomalacia (softening of the bones)
- Muscle pain
- Weakness
Other symptoms can include:
- Decreased urine output
- Increased heart rate or irregular heartbeat
- Muscle cramps
- Pain in the bones, back, flank, or abdomen
- Skeletal deformities
Exams and Tests
The health care provider will perform a physical exam and ask about the symptoms.
Tests that may be ordered include:
- Arterial blood gas
- Blood chemistry
- Blood pH level
- Urine pH and acid-loading test
- Urinalysis
Treatment
The goal is to restore normal acid level and electrolyte balance in the body. This will help correct bone disorders and reduce the risk for osteomalacia and osteopenia in adults.
Some adults may need no treatment. All children need alkaline medicine such as potassium citrate and sodium bicarbonate. This is medicine that helps correct the acidic condition of the body. The medicine helps prevent bone disease caused by too much acid, such as rickets, and to allow normal growth.
Thiazide diuretics are also frequently used to preserve bicarbonate in the body.
The underlying cause of proximal renal tubular necrosis should be corrected if it can be found.
Vitamin D and calcium supplements may be needed to help reduce skeletal deformities resulting from osteomalacia.
Outlook (Prognosis)
Although the underlying cause of proximal renal tubular acidosis may go away by itself, the effects and complications can be permanent or life threatening. Treatment is usually successful.
When to Contact a Medical Professional
Contact your provider if you have symptoms of proximal renal tubular acidosis.
Get medical help right away if any of the following emergency symptoms develop:
- Decreased alertness or disorientation
- Decreased consciousness
- Seizures
Prevention
Most of the disorders that cause proximal renal tubular acidosis are not preventable.
References
Bushinsky DA. Kidney stones. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 32.
Dixon BP. Renal tubular acidosis. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 569.
Seifter JL. Acid-base disorders. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 104.
Review Date: 12/31/2023
Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.