Infectious esophagitis
Infection - esophagus; Esophageal infection
Esophagitis is a term for any inflammation, irritation, or swelling of the esophagus. This is the tube that carries food and liquids from the mouth to the stomach.
Infectious esophagitis is an infection of the esophagus from viruses, bacteria, fungi, or yeast. This most often occurs in people with a weak immune system.
Causes
Infectious esophagitis is rare. It often occurs in people with weak immune systems. People who have strong immune systems don't usually develop the infection.
Common causes of a weakened immune system include:
- HIV/AIDS
- Chemotherapy
- Diabetes
- Leukemia or lymphoma
- Medicines that suppress the immune system, such as ones given after organ or bone marrow transplant
- Other conditions that suppress or weaken your immune system
Organisms (germs) that cause esophagitis include fungi, yeast, and viruses. Common organisms include:
- Candida albicans and other Candida species
- Cytomegalovirus (CMV)
- Herpes simplex virus (HSV)
- Human papillomavirus (HPV)
- Tuberculosis bacteria (Mycobacterium tuberculosis) -- not common
Symptoms
Symptoms of infectious esophagitis include:
- Difficulty swallowing
- Painful swallowing
- Fever and chills
- Yeast infection of the tongue and lining of the mouth (oral thrush)
- Sores in the mouth or back of the throat (with herpes or CMV)
Exams and Tests
Your health care provider will ask about your symptoms and examine your mouth and throat. Tests may include:
- Blood and urine tests for CMV
- Culture of cells from the esophagus for herpes or CMV
- Mouth or throat swab culture for candida
You may need to have an upper endoscopy exam. This is a test to examine the lining of the esophagus.
Treatment
Most often, medicines can control the infection. The type of medicine given will depend on the cause of the infection.
Antiviral medicines can treat a herpes infection. Common antiviral medicines for a herpes infection are:
- Acyclovir
- Famciclovir
- Valacyclovir
Antifungal medicines can treat candida infection. Common antifungal medicines are:
- Fluconazole (taken by mouth)
- Caspofungin (given by injection)
- Amphotericin (given by injection)
Antiviral medicines can treat CMV infection. Ganciclovir or foscarnet are given through a vein (intravenously). In some cases, a medicine called valganciclovir, which is taken by mouth, can be used for CMV infection.
Some people may also need pain medicine.
Ask your provider for special diet recommendations. For example, there may be foods you need to avoid eating as your esophagitis heals.
Many people need other long-term medicines to suppress the virus or fungus and to prevent the infection from coming back.
Outlook (Prognosis)
In people with a healthy immune system, esophagitis often goes away on its own. People with a weak immune system may take longer to get better.
Possible Complications
Health problems that may result from infectious esophagitis include:
- Holes in your esophagus (perforations)
- Infection at other sites
- Recurrent infection
When to Contact a Medical Professional
Contact your provider if you have any condition that can cause reduced immune response and you develop symptoms of infectious esophagitis.
Prevention
If you have a weak immune system, try to avoid contact with people who have an infection with any of the organisms mentioned above.
References
Graman PS. Esophagitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 97.
Katzka DA. Esophageal disorders caused by medications, trauma, and infection. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 45.
Herpetic esophagitis - illustration
Herpetic esophagitis
illustration
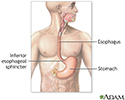
Upper gastrointestinal system - illustration
Upper gastrointestinal system
illustration
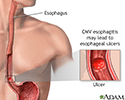
CMV esophagitis - illustration
CMV esophagitis
illustration
Candidal esophagitis - illustration
Candidal esophagitis
illustration
Review Date: 8/26/2023
Reviewed By: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.