Pneumocystis jirovecii pneumonia
Pneumocystis pneumonia; Pneumocystosis; PCP; Pneumocystis carinii; PJP pneumonia
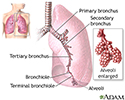
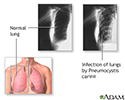
Pneumocystis jirovecii pneumonia is a fungal infection of the lungs. The disease used to be called Pneumocystis carinii or PCP pneumonia.
Causes
This type of pneumonia is caused by the fungus Pneumocystis jirovecii. This fungus is common in the environment and rarely causes illness in healthy people.
However, it can cause a lung infection in people with a weakened immune system due to:
- Cancer
- Long-term use of corticosteroids or other medicines that weaken the immune system
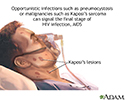
- HIV/AIDS
- Organ or bone marrow transplantation
Pneumocystis jirovecii was a rare infection before the AIDS epidemic. Before the use of preventive antibiotics for the condition, most people in the United States with advanced AIDS developed this infection.
Symptoms
Pneumocystis pneumonia in people with AIDS usually develops slowly over days to weeks or even months, and is less severe. People with pneumocystis pneumonia who do not have AIDS usually get sick faster and are more severely ill.
Symptoms include:
- Cough, often mild and dry
- Fever
- Rapid breathing
- Shortness of breath, especially with activity (exertion)
Exams and Tests
Your health care provider will examine you and ask about your symptoms.
Tests that may be ordered include:
- Blood gases (both arterial and venous)
- Bronchoscopy (with lavage)
- Lung biopsy
- X-ray of the chest
- Sputum exam to check for fungus that causes the infection
- Complete blood count (CBC)
- Beta-1,3 glucan level in the blood and/or lavage fluid from bronchoscopy
Treatment
Anti-infection medicines can be given by mouth (orally) or through a vein (intravenously), depending on how severe the illness is.
People with low oxygen levels and moderate to severe disease are often prescribed corticosteroids as well.
Outlook (Prognosis)
Pneumocystis pneumonia can be life threatening. It can cause respiratory failure that can lead to death. People with this condition need early and effective treatment. For moderate to severe pneumocystis pneumonia in people with HIV/AIDS, the short term use of corticosteroids has decreased the incidence of death.
Possible Complications
Complications that may result include:
- Pleural effusion (extremely rare)
- Pneumothorax (collapsed lung)
- Respiratory failure (may require breathing support)
When to Contact a Medical Professional
If you have a weakened immune system due to AIDS, cancer, transplantation, or corticosteroid use, contact your provider if you develop a cough, fever, or shortness of breath.
Prevention
Preventive therapy is recommended for:
- People with HIV/AIDS who have CD4 counts below 200 cells/microliter or 200 cells/cubic millimeter
- Bone marrow transplant recipients
- Organ transplant recipients
- People who take long-term, high-dose corticosteroids
- People who have had previous episodes of this infection
- People who take long-term immunomodulatory medicines
References
Kovacs JA. Pneumocystis pneumonia. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 313.
Miller RF Walzer PD, Smulian AG. Pneumocystis species. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 269.
Review Date: 12/31/2023
Reviewed By: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.