Chronic motor or vocal tic disorder
Chronic vocal tic disorder; Tic - chronic motor tic disorder; Persistent (chronic) motor or vocal tic disorder; Chronic motor tic disorder
Chronic motor or vocal tic disorder is a condition that involves quick, uncontrollable movements or vocal outbursts (but not both).
Causes
Chronic motor or vocal tic disorder is more common than Tourette syndrome. Chronic tics may be forms of Tourette syndrome. Tics usually start at age 5 or 6 and get worse until age 12. They often improve during adulthood.
Symptoms
A tic is a sudden, fast, repeated movement or sound that has no reason or goal. Tics can involve:
- Excessive blinking
- Grimaces of the face
- Quick movements of the arms, legs, or other areas
- Sounds (grunts, throat clearing, contractions of the abdomen or diaphragm)
Some people have many kinds of tics.
People with the condition can hold off these symptoms for a short time. But they feel relief when they carry out these movements. They often describe the tics as a response to an inner urge. Some say they have abnormal sensations in the area of the tic before it occurs.
Tics may continue during all stages of sleep, though may be less frequent. They may get worse with:
- Excitement
- Fatigue
- Heat
- Stress
Exams and Tests
Your health care provider can usually diagnose a tic during a physical examination. Tests are generally not needed.
People are diagnosed with the disorder when:
- They have had the tics for more than a year
- There is no other medical problem or substance use causing the symptoms
Treatment
Treatment depends on how severe the tics are and how the condition affects you. Medicines and talk therapy (cognitive behavioral therapy) are used when the tics greatly affect daily activities, such as school and job performance.
Medicines can help control or reduce tics. But they have side effects, such as movement and thinking problems.
Outlook (Prognosis)
Children who develop this disorder between ages 6 and 8 often do very well. Symptoms may last 4 to 6 years, and then stop in the early teens without treatment.
When the disorder begins in older children and continues into the 20s, it may become a lifelong condition.
Possible Complications
There are usually no complications.
When to Contact a Medical Professional
There is usually no need to see your provider for a tic unless it is severe or disrupts daily life.
If you cannot tell whether you or your child's movements are a tic or something more serious (such as a seizure), contact your provider.
References
Kim JW, Walter HJ, DeMaso DR. Motor disorders and habits. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 37.
Singer HS, Mink JW, Gilbert DL, Jankovic J. Tics and tourette syndrome. In: Singer HS, Mink JW, Gilbert DL, Jankovic J, eds. Movement Disorders in Childhood. 3rd ed. Philadelphia, PA: Elsevier; 2022:chap 7.
Tochen L, Singer HS. Tics and Tourette syndrome. In: Swaiman KF, Ashwal S, Ferriero DM, et al, eds. Swaiman's Pediatric Neurology: Principles and Practice. 6th ed. Philadelphia, PA: Elsevier; 2017:chap 98.
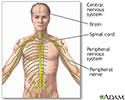
Central nervous system and peripheral nervous system - illustration
Central nervous system and peripheral nervous system
illustration
Brain - illustration
Brain
illustration
Brain and nervous system - illustration
Brain and nervous system
illustration
Brain structures - illustration
Brain structures
illustration
Central nervous system and peripheral nervous system - illustration
Central nervous system and peripheral nervous system
illustration
Brain - illustration
Brain
illustration
Brain and nervous system - illustration
Brain and nervous system
illustration
Brain structures - illustration
Brain structures
illustration
Review Date: 3/31/2024
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.