Autoimmune disorders
An autoimmune disorder occurs when the body's immune system attacks and destroys healthy body tissue by mistake. There are more than 80 autoimmune disorders.
The blood cells in the body's immune system help protect against harmful substances. Examples include bacteria, viruses, toxins, cancer cells, and blood and tissue from outside the body. These substances contain antigens. The immune system produces antibodies against these antigens that enable it to destroy these harmful substances.
When you have an autoimmune disorder, your immune system does not distinguish between healthy tissue and potentially harmful antigens. As a result, your body sets off a reaction that destroys normal tissues.
The exact cause of autoimmune disorders is unknown. One theory is that some microorganisms (such as bacteria or viruses) or drugs may trigger changes that confuse the immune system. This may happen more often in people who have genes that make them more prone to autoimmune disorders.
An autoimmune disorder may result in:
- The destruction of body tissue
- Abnormal growth of an organ
- Changes in organ function
An autoimmune disorder may affect one or more organ or tissue types. Areas often affected by autoimmune disorders include:
- Blood vessels
- Connective tissues
- Endocrine glands such as the thyroid or pancreas
- Joints
- Muscles
- Red blood cells
- Skin
A person may have more than one autoimmune disorder at the same time. Common autoimmune disorders include:
- Addison disease
- Celiac disease - sprue (gluten-sensitive enteropathy)
- Dermatomyositis
- Graves disease
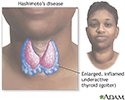
- Hashimoto thyroiditis
- Inflammatory bowel disease (Crohn disease, ulcerative colitis)
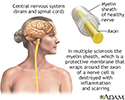
- Multiple sclerosis
- Myasthenia gravis
- Pernicious anemia
- Reactive arthritis
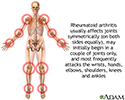
- Rheumatoid arthritis
- Sjögren syndrome
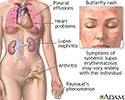
- Systemic lupus erythematosus (lupus)
- Type I diabetes
Symptoms
Symptoms will vary, based on the type and location of the faulty immune response. Common symptoms include:
Exams and Tests
Your health care provider will do a physical exam. Signs depend on the type of disease.
Tests that may be done to diagnose an autoimmune disorder include:
- Antinuclear antibody (ANA) tests
- Autoantibody tests
- Complete blood count (CBC) with white blood cell differential (CBC with WBC differential)
- Comprehensive metabolic panel
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Urinalysis
Treatment
The goals of treatment are to:
- Control the autoimmune process
- Maintain your body's ability to fight disease
- Reduce symptoms
Treatments will depend on your disease and symptoms. Types of treatments include:
- Supplements to replace a substance that the body lacks, such as thyroid hormone, vitamin B12, or insulin, due to the autoimmune disease
- Blood transfusions if blood is affected
- Physical therapy to help with movement if the bones, joints, or muscles are affected
Many people take medicines to reduce the immune system's abnormal response. These are called immunosuppressive medicines. Examples include corticosteroids (such as prednisone) and nonsteroid drugs such as azathioprine, cyclophosphamide, mycophenolate, sirolimus, or tacrolimus. Targeted drugs such as tumor necrosis factor (TNF) blockers and Interleukin inhibitors can be used for some diseases.
Outlook (Prognosis)
The outcome depends on the disease. Most autoimmune diseases are chronic, but many can be controlled with treatment.
Symptoms of autoimmune disorders can come and go. When symptoms get worse, it is called a flare-up.
Possible Complications
Complications depend on the disease. Medicines used to suppress the immune system can cause severe side effects, such as higher risk for infections.
When to Contact a Medical Professional
Contact your provider if you develop symptoms of an autoimmune disorder.
Prevention
There is no known prevention for most autoimmune disorders.
References
Kono DH, Theofilopoulos AN. Autoimmunity and tolerance. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 22.
Kumar V, Abbas AK, Aster JC. Diseases of the immune system. In: Kumar V, Abbas AK, Aster JC, eds. Robbins and Cotran Pathologic Basis of Disease. 10th ed. Philadelphia, PA: Elsevier; 2021:chap 6.
Peakman M, Buckland MS. The immunity. In: Feather A, Randall D, Waterhouse M, eds. Kumar and Clarke's Clinical Medicine. 10th ed. Philadelphia, PA: Elsevier; 2021:chap 3.
Graves disease - illustration
Graves disease
illustration
Hashimoto's disease (chronic thyroiditis) - illustration
Hashimoto's disease (chronic thyroiditis)
illustration
Multiple sclerosis - illustration
Multiple sclerosis
illustration
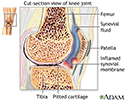
Rheumatoid arthritis - illustration
Rheumatoid arthritis
illustration
Rheumatoid arthritis - illustration
Rheumatoid arthritis
illustration
Systemic lupus erythematosus - illustration
Systemic lupus erythematosus
illustration
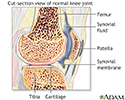
Synovial fluid - illustration
Synovial fluid
illustration
Rheumatoid arthritis - illustration
Rheumatoid arthritis
illustration
Antibodies - illustration
Antibodies
illustration
Graves disease - illustration
Graves disease
illustration
Hashimoto's disease (chronic thyroiditis) - illustration
Hashimoto's disease (chronic thyroiditis)
illustration
Multiple sclerosis - illustration
Multiple sclerosis
illustration
Rheumatoid arthritis - illustration
Rheumatoid arthritis
illustration
Rheumatoid arthritis - illustration
Rheumatoid arthritis
illustration
Systemic lupus erythematosus - illustration
Systemic lupus erythematosus
illustration
Synovial fluid - illustration
Synovial fluid
illustration
Rheumatoid arthritis - illustration
Rheumatoid arthritis
illustration
Antibodies - illustration
Antibodies
illustration
Review Date: 6/12/2023
Reviewed By: Jacob Berman, MD, MPH, Clinical Assistant Professor of Medicine, Division of General Internal Medicine, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.