Ectopic pregnancy
Tubal pregnancy; Cervical pregnancy; Tubal ligation - ectopic pregnancy
An ectopic pregnancy is a pregnancy that occurs outside the womb (uterus).
Causes
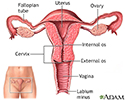
In most pregnancies, the fertilized egg travels through the fallopian tube to the womb (uterus). If the movement of the egg is blocked or slowed through the tubes, it can lead to an ectopic pregnancy. Things that may cause this problem include:
- Birth defect in the fallopian tubes
- Scarring after a ruptured appendix
- Endometriosis
- Having had an ectopic pregnancy in the past
- Scarring from past infections or surgery of the female organs
- History of prior abdominal surgery
The following also increase risk for an ectopic pregnancy:
- Age over 35
- Getting pregnant while having an intrauterine device (IUD)
- Having your fallopian tubes tied
- Having had surgery to untie fallopian tubes to become pregnant
- Having had many sexual partners
- Sexually transmitted infections (STI)
- Some infertility treatments
Sometimes, the cause is not known. Hormones may play a role.
The most common site for an ectopic pregnancy is the fallopian tube. In rare cases, this can occur in the ovary, abdomen, or cervix.
An ectopic pregnancy can occur even if you use birth control.
Symptoms
Symptoms of ectopic pregnancy may include:
- Abnormal vaginal bleeding
- Mild cramping on one side of the pelvis
- No periods
- Pain in the lower belly or pelvic area
If the area around the abnormal pregnancy ruptures and bleeds, symptoms may get worse. They may include:
- Fainting or feeling faint
- Intense pressure in the rectum
- Low blood pressure
- Pain in the shoulder area
- Severe, sharp, and sudden pain in the lower abdomen
Exams and Tests
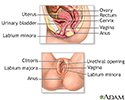
The health care provider will do a pelvic exam. The exam may show tenderness in the pelvic area.
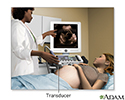
A pregnancy test and vaginal ultrasound will be done.
Human chorionic gonadotropin (hCG) is a hormone that is produced during pregnancy. Checking the blood level of this hormone can detect pregnancy.
- When hCG levels are above a certain value, a pregnancy sac in the uterus should be seen with ultrasound.
- If the sac is not seen, this may indicate that an ectopic pregnancy is present.
You may need more than one exam, ultrasound, and blood test. Your provider will instruct you about signs to watch for until your next visit.
Treatment
Ectopic pregnancy may be life threatening. The pregnancy cannot continue to birth (term). Effective treatment requires either medical treatment to end the pregnancy or surgical removal of the pregnancy.
If the ectopic pregnancy has not ruptured, treatment may include:
- Surgery
- Medicine that ends the pregnancy, along with close monitoring by your provider
You will need emergency medical help if the area of the ectopic pregnancy breaks open (ruptures). Rupture can lead to bleeding and shock. Treatment for shock may include:
- Blood transfusion
- Fluids given through a vein
- Keeping warm
- Oxygen
- Raising the legs
If there is a rupture, surgery is done to stop blood loss and remove the pregnancy. In some cases, the surgeon may have to remove the fallopian tube.
Outlook (Prognosis)
If diagnosed early, treatment is very effective. It's important to seek early care whenever you believe you may be pregnant so your provider may determine the location of the pregnancy.
One out of three women who have had one ectopic pregnancy can have a baby in the future. Another ectopic pregnancy is more likely to occur. Some women do not become pregnant again.
The likelihood of a successful pregnancy after an ectopic pregnancy depends on:
- The woman's age
- Whether she has already had children
- Why the first ectopic pregnancy occurred
- The health of her fallopian tubes
When to Contact a Medical Professional
Contact your provider if you have:
- Abnormal vaginal bleeding
- Lower abdominal or pelvic pain or
- Suspect you might be pregnant
Prevention
Most forms of ectopic pregnancy that occur outside the fallopian tubes are probably not preventable. You may be able to reduce your risk by avoiding conditions that may scar the fallopian tubes. These steps include:
- Practicing safer sex by taking steps before and during sex, which can prevent you from getting an infection
- Getting early diagnosis and treatment of all STIs
- Stopping smoking
References
Alur-Gupta S, Cooney LG, Senapati S, Sammel MD, Barnhart KT. Two-dose versus single-dose methotrexate for treatment of ectopic pregnancy: a meta-analysis. Am J Obstet Gynecol. 2019;221(2):95-108.e2. PMID: 30629908 pubmed.ncbi.nlm.nih.gov/30629908/.
Henn MC, Lall MD. Complications of pregnancy. In: Walls RM, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 173.
Hur HC, Lobo RA. Ectopic pregnancy: etiology, pathology, diagnosis, management, fertility prognosis. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 17.
Nelson AL, Gambone JC. Ectopic pregnancy. In: Hacker NF, Gambone JC, Hobel CJ, eds. Hacker & Moore's Essentials of Obstetrics and Gynecology. 6th ed. Philadelphia, PA: Elsevier; 2016:chap 24.
Pelvic laparoscopy - illustration
Pelvic laparoscopy
illustration
Ultrasound in pregnancy - illustration
Ultrasound in pregnancy
illustration
Female reproductive anatomy - illustration
Female reproductive anatomy
illustration
Uterus - illustration
Uterus
illustration
Ectopic pregnancy - illustration
Ectopic pregnancy
illustration
Pelvic laparoscopy - illustration
Pelvic laparoscopy
illustration
Ultrasound in pregnancy - illustration
Ultrasound in pregnancy
illustration
Female reproductive anatomy - illustration
Female reproductive anatomy
illustration
Uterus - illustration
Uterus
illustration
Ectopic pregnancy - illustration
Ectopic pregnancy
illustration
Review Date: 3/31/2024
Reviewed By: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.