Placenta previa
Vaginal bleeding - placenta previa; Pregnancy - placenta previa
Placenta previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix.
The placenta grows during pregnancy and feeds the developing baby. The cervix is the opening to the birth canal.
Causes
During pregnancy, the placenta moves as the womb stretches and grows. It is very common for the placenta to be low in the womb in early pregnancy. But as the pregnancy continues, the placenta moves to the top of the womb. By the third trimester, the placenta should be near the top of the womb, so the cervix is open for delivery.
Sometimes, the placenta partly or completely covers the cervix. This is called a placenta previa.
There are different forms of placenta previa:
- Marginal: The placenta is next to the cervix but does not cover the opening.
- Partial: The placenta covers part of the cervical opening.
- Complete: The placenta covers all of the cervical opening.
Placenta previa occurs in 1 out of 200 pregnancies. It is more common in women who have:
- An abnormally shaped uterus
- Had many pregnancies in the past
- Had multiple pregnancies, such as twins or triplets
- Scarring on the lining of the uterus due to a history of surgery, C-section, or abortion
- In vitro fertilization
- A history of placenta previa in a previous pregnancy
Women who smoke, use cocaine, or have their children at an older age may also have an increased risk.
Symptoms
The main symptom of placenta previa is sudden bleeding from the vagina. Some women also have cramps. The bleeding often starts near the end of the second trimester or beginning of the third trimester.
Bleeding may be severe and life threatening. It may stop on its own but can start again days or weeks later.
Labor sometimes starts within several days of the heavy bleeding. Sometimes, bleeding may not occur until after labor starts.
Exams and Tests
Your health care provider can diagnose this condition with a pregnancy ultrasound.
Treatment
Your provider will carefully consider the risk of bleeding against early delivery of your baby. After 36 weeks, delivery of the baby may be the best treatment.
Nearly all women with placenta previa will need a C-section. If the placenta covers all or part of the cervix, a vaginal delivery can cause severe bleeding. This can be deadly to both the mother and baby.
If the placenta is near or covering part of the cervix, your provider may recommend:
- Reducing your activities
- Bed rest
- Pelvic rest, which means no sex, no tampons, and no douching
Nothing should be placed in your vagina.
You may need to stay in the hospital so your health care team can closely monitor you and your baby.
Other treatments you may receive:
- Blood transfusions
- Medicines to prevent early labor
- Medicines to help pregnancy continue to at least 36 weeks
- Shot of special medicine called Rhogam if your blood type is Rh-negative
- Steroid shots to help the baby's lungs mature
An emergency C-section may be done if the bleeding is heavy and cannot be controlled.
Outlook (Prognosis)
The biggest risk is severe bleeding that can be life threatening to the mother and baby. If you have severe bleeding, your baby may need to be delivered early, before major organs, such as the lungs, have developed.
For most women who receive regular prenatal care, this condition is diagnosed before symptoms appear. This helps the provider and mother take steps to minimize risks from this condition.
When to Contact a Medical Professional
Contact your provider if you have vaginal bleeding during pregnancy. Placenta previa can be dangerous to both you and your baby.
References
Francois KE, Foley MR. Antepartum and postpartum hemorrhage. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Hull AD, Resnik R, Silver RM. Placenta previa and accreta, vasa previa, subchorionic hemorrhage, and abruptio placentae. In: Lockwood CJ, Copel JA, Dugoff L, et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2023:chap 43.
Henn MC, Lall MD. Complications of pregnancy. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 173.
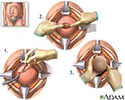
C-section
Animation
Cesarean section - illustration
Cesarean section
illustration
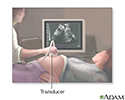
Ultrasound in pregnancy - illustration
Ultrasound in pregnancy
illustration
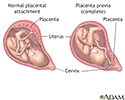
Anatomy of a normal placenta - illustration
Anatomy of a normal placenta
illustration
Placenta previa - illustration
Placenta previa
illustration
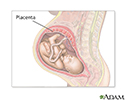
Placenta - illustration
Placenta
illustration
Ultrasound, normal fetus - arms and legs - illustration
Ultrasound, normal fetus - arms and legs
illustration
Ultrasound, normal relaxed placenta - illustration
Ultrasound, normal relaxed placenta
illustration
Ultrasound, color - normal umbilical cord - illustration
Ultrasound, color - normal umbilical cord
illustration
Placenta - illustration
Placenta
illustration
Cesarean section - illustration
Cesarean section
illustration
Ultrasound in pregnancy - illustration
Ultrasound in pregnancy
illustration
Anatomy of a normal placenta - illustration
Anatomy of a normal placenta
illustration
Placenta previa - illustration
Placenta previa
illustration
Placenta - illustration
Placenta
illustration
Ultrasound, normal fetus - arms and legs - illustration
Ultrasound, normal fetus - arms and legs
illustration
Ultrasound, normal relaxed placenta - illustration
Ultrasound, normal relaxed placenta
illustration
Ultrasound, color - normal umbilical cord - illustration
Ultrasound, color - normal umbilical cord
illustration
Placenta - illustration
Placenta
illustration
Review Date: 4/16/2024
Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.