Kneecap dislocation
Dislocation - kneecap; Patellar dislocation or instability
Kneecap dislocation occurs when the round-shaped bone covering the knee (patella) moves or slides out of place. The dislocation often occurs toward the outside of the leg.
Causes
Kneecap dislocation often occurs after a sudden change in direction when your leg is planted. This puts your kneecap under stress. This can occur when playing certain sports, such as basketball.
Dislocation may also occur as result of direct trauma. When the kneecap is dislocated, it can slip sideways to the outside of the knee.
Symptoms
Symptoms of kneecap dislocation include:
- Knee appears to be deformed
- Knee is bent and cannot be straightened out
- Kneecap (patella) dislocates to the outside of the knee
- Knee pain and tenderness
- Knee swelling
- "Sloppy" kneecap -- you can move the kneecap too much from right to left (hypermobile patella)
The first few times this occurs, you will feel pain and may be unable to walk. If you continue to have dislocations, your knee may not hurt as much and you may not be as disabled. This is not a reason to avoid treatment. Kneecap dislocation damages your knee joint. It can lead to cartilage injuries and increase the risk of developing osteoarthritis at a younger age. Repeat dislocations will make the condition worse and harder to treat.
First Aid
If you can, straighten out your knee. If it is stuck and painful to move, stabilize (splint) the knee and get medical attention.
Your health care provider will examine your knee. This may confirm that the kneecap is dislocated. If it is, your provider will reduce (relocate) your dislocation.
Your provider may order a knee x-ray or an MRI. These tests can show if the dislocation caused a broken bone or cartilage damage. If tests show that you have no damage, your knee will be placed into a knee brace immobilizer to prevent you from moving it. You will need to wear this for about 3 weeks.
Once you are no longer in the brace, physical therapy can help build back your muscle strength and improve the knee's range of motion.
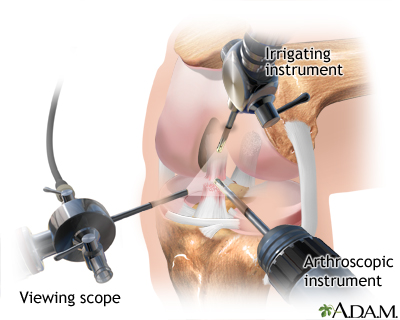
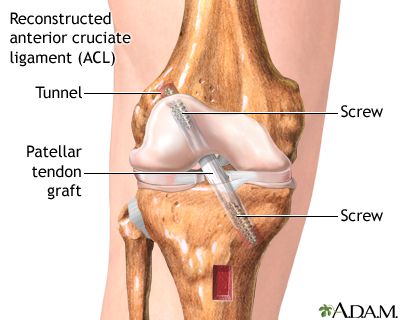
If there is damage to the bone and cartilage, or if the kneecap continues to be unstable, you may need surgery to stabilize the kneecap. This may be done using arthroscopic or open surgery.
When to Contact a Medical Professional
Contact your provider if you injure your knee and have symptoms of dislocation.
Contact your provider if you are being treated for a dislocated knee and you notice:
- Increased instability in your knee
- Pain or swelling return after they went away
- Your injury does not appear to be getting better with time
Also contact your provider if you re-injure your knee.
Prevention
Use proper techniques when exercising or playing sports. Keep your knees strong and flexible.
Some cases of knee dislocation may not be preventable, especially if physical factors make you more likely to dislocate your knee.
References
Mascioli AA. Acute dislocations. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 60.
Naples RM, Ufberg JW. Management of common dislocations. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges' Clinical Procedures in Emergency Medicine and Acute Care. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 49.
Sherman SL, Hinckel BB, Farr J. Patellar instability. In: Miller MD, Thompson SR, eds. DeLee, Drez, & Miller's Orthopaedic Sports Medicine. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 105.
Arthroscopy - illustration
Arthroscopy
illustration
Patellar dislocation - illustration
Patellar dislocation
illustration
Knee arthroscopy - series - Normal anatomy
Presentation
Review Date: 12/12/2022
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.