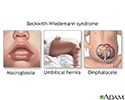
Beckwith-Wiedemann syndrome
Beckwith-Wiedemann syndrome is a growth disorder that causes large body size, large organs, and other symptoms. It is a congenital condition, which means it is present at birth. The signs and symptoms of the disorder vary somewhat from child to child.
Infancy can be a critical period in babies with this condition because of the possibility of:
- Low blood sugar (hypoglycemia)
- A type of hernia called an omphalocele (when present)
- An enlarged tongue (macroglossia)
- An increased rate of tumor growth. Wilms tumors and hepatoblastomas are the most common tumors in children with this syndrome.
Beckwith-Wiedemann syndrome is caused by a defect in the genes on chromosome 11. About 10% of cases are passed down through families.
Symptoms
Signs and symptoms of Beckwith-Wiedemann syndrome include:
- Large size for a newborn
- Red birth mark on forehead or eyelids (nevus flammeus)
- Creases in ear lobes
- Large tongue (macroglossia)
- Low blood sugar (hypoglycemia)
- Abdominal wall defect (umbilical hernia or omphalocele)
- Enlargement of some organs
- Overgrowth of one side of the body (hemihyperplasia/hemihypertrophy)
- Tumor growth, such as Wilms tumors and hepatoblastomas
Exams and Tests
The health care provider will do a physical exam to look for signs and symptoms of Beckwith-Wiedemann syndrome. Often this is enough to make a diagnosis.
Tests for the disorder include:
- Blood tests for low blood sugar
- Chromosomal studies for abnormalities in chromosome 11
- Ultrasound of the abdomen
Treatment
Infants with low blood sugar may be treated with fluids given through a vein (intravenous, IV). Some infants may need medicine or other management if low blood sugar continues.
Defects in the abdominal wall may need to be repaired. If the enlarged tongue makes it hard to breathe or eat, surgery may be needed. Children with overgrowth on one side of the body should be watched for a curved spine (scoliosis). The child also must be watched closely for the development of tumors. Tumor screening includes blood tests and abdominal ultrasounds.
Outlook (Prognosis)
Children with Beckwith-Wiedemann syndrome typically lead normal lives. Further study is needed to develop long-term follow-up information.
Possible Complications
These complications can occur:
- Development of tumors
- Feeding problems due to enlarged tongue
- Breathing problems due to enlarged tongue
- Scoliosis due to hemihypertrophy
When to Contact a Medical Professional
If you have a child with Beckwith-Wiedemann syndrome and worrisome symptoms develop, contact your pediatrician right away.
Prevention
There is no known prevention for Beckwith-Wiedemann syndrome. Genetic counseling may be of value for families who would like to have more children.
References
Garg M, Devaskar SU. Disorders of carbohydrate metabolism in the neonate. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 86.
Madan-Khetarpal S, Arnold G, Ortiz D. Genetic disorders and dysmorphic conditions. In: Zitelli BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 1.
Sperling MA. Hypoglycemia. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 111.
Review Date: 4/28/2023
Reviewed By: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.