Vasectomy
Sterilization surgery - male; No-scalpel vasectomy; NSV; Family planning - vasectomy; Contraception - vasectomy
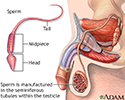
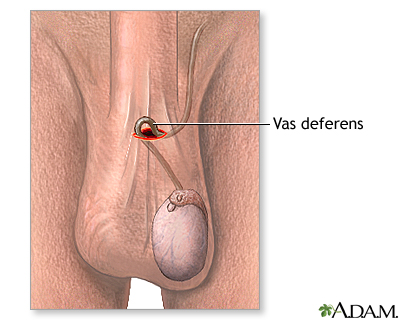
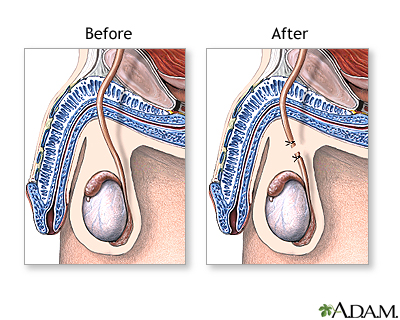
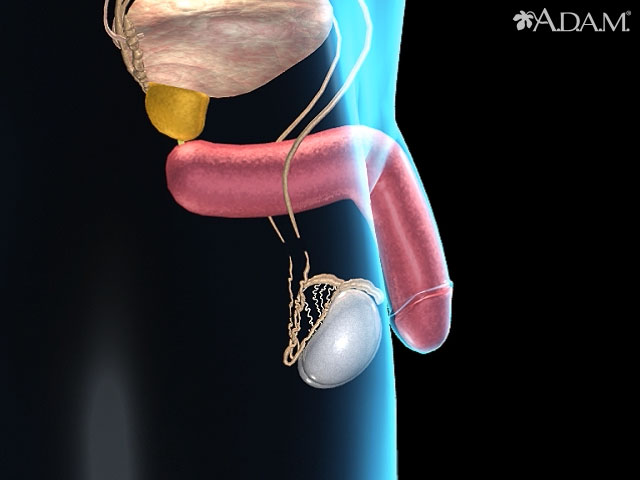
A vasectomy is surgery to cut the vas deferens. These are the tubes that carry sperm from the testicles to the urethra. After a vasectomy, sperm cannot move out of the testes. A man who has had a successful vasectomy cannot make a woman pregnant.
Description
Vasectomy is most often done in the surgeon's office using local anesthesia. You will be awake, but not feel any pain.
- After your scrotum is shaved and cleaned, the surgeon will inject numbing medicine into the area.
- The surgeon will make a small cut in the upper part of your scrotum. The vas deferens will then be tied off or clipped and cut apart.
- The wound will be closed with stitches or surgical glue.
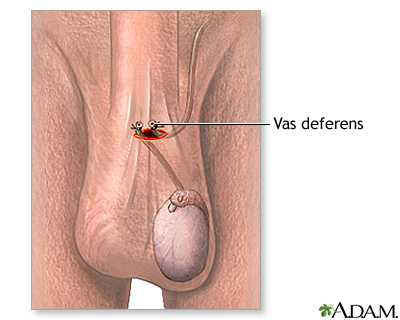
You may have a vasectomy without a surgical cut. This is called a no-scalpel vasectomy (NSV). For this procedure:
- The surgeon will find the vas deferens by feeling your scrotum.
- You will get numbing medicine.
- The surgeon will then make a tiny hole in the skin of your scrotum and then tie off and cut a part of the vas deferens.
In a regular vasectomy, a small incision is made on each side of the scrotum. In a no-scalpel vasectomy, a sharp instrument is used to pierce the skin and make a single opening. A stitch or surgical glue is used to seal the openings in both forms of the procedure.
Why the Procedure Is Performed
Vasectomy may be recommended for men who are sure they do not want to get a woman pregnant in the future. A vasectomy makes a man sterile (unable to get a woman pregnant).
A vasectomy is not recommended as a short-term form of birth control. The procedure to reverse a vasectomy is a much more complicated operation and may not be covered by insurance.
Vasectomy may be a good choice for a man who:
- Is in a relationship, and both partners agree that they do not want children or additional children. They do not want to use, or cannot use, other forms of birth control.
- Is in a relationship and a pregnancy would be unsafe for the woman partner because of health problems.
- Is in a relationship, and one or both partners have genetic disorders that they do not want to pass on.
- Does not want to be bothered by having to use other forms of birth control during sexual activity.
Vasectomy may not be a good choice for a man who:
- Is in a relationship with someone who has not decided on whether to have children in the future.
- Is in an unstable or stressful relationship.
- Is considering the operation just to please a partner.
- Wants to have children later by storing sperm or by reversing the vasectomy.
- Is young and may want to make a different decision in the future.
- Is single when deciding to have a vasectomy. This includes men who are divorced, widowed, or separated.
Risks
There is no serious risk to vasectomy. Your semen will be tested in the months after the operation to make sure it does not contain sperm.
As with any surgical procedure, infection, swelling, or prolonged pain can occur. Careful following of aftercare instructions reduces these risks significantly.
Very rarely, the vas deferens can grow back together again. If this happens, sperm can mix with semen. This would make it possible for you to make a woman pregnant.
Before the Procedure
Two weeks before your vasectomy, tell your health care provider about medicines you take, including those bought without a prescription and vitamins, supplements, and herbs.
You may need to limit or stop taking aspirin, ibuprofen (Advil, Motrin), and other medicines that affect blood clotting for 10 days before your surgery.
On the day of your surgery, wear loose, comfortable clothes. Clean your scrotum area well. Take the medicines your provider told you to take.
Bring a scrotal support with you to the surgery.
After the Procedure
You should be able to return home as soon as you feel well. You can return to work the next day if you do not do heavy physical work. Most men return to work within 2 to 3 days. You should be able to return to your normal physical activities in 3 to 7 days. It is normal to have some swelling and bruising of the scrotum after the procedure. It should go away within 2 weeks.
You should wear a scrotal support for 3 to 4 days after the procedure. You can use an ice pack to reduce swelling. Pain medicine, such as acetaminophen (Tylenol), may help relieve discomfort. You can have sexual intercourse as soon as you feel ready, most often about a week after the surgery. You must use some form of birth control to prevent unwanted pregnancy until you know your semen is free of sperm.
The vasectomy is considered successful only after your semen has been tested to make sure no more sperm are in it. It is safe to stop using other forms of birth control at this point.
Outlook (Prognosis)
Vasectomy does not affect a man's ability to have an erection or orgasm, or to ejaculate semen. A vasectomy does not prevent the spread of sexually transmitted infections (STIs).
A vasectomy does not increase your risk of prostate cancer or testicular disease.
Your sperm count gradually decreases after a vasectomy. After about 3 months, sperm are no longer present in the semen. You must continue to use birth control to prevent pregnancy until your semen sample is totally free of sperm.
Most men are satisfied with vasectomy. Most couples enjoy not having to use birth control.
References
Brugh VM. Vasectomy. In: Smith JA Jr, Howards SS, Preminger GM, Dmochowski RR, eds. Hinman's Atlas of Urologic Surgery. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 110.
Hawksworth DJ, Khera M, Herati AS. Surgery of the scrotum and seminal vesicles. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 83.
Wilson CL. Vasectomy. In: Fowler GC, ed. Pfenninger and Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 111.
Review Date: 3/31/2024