Severe acute respiratory syndrome (SARS)
SARS; Respiratory failure - SARS; SARS coronavirus; SARS-CoV
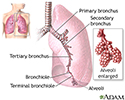
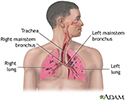
Severe acute respiratory syndrome (SARS) is a serious form of pneumonia. Infection with the SARS virus causes acute respiratory distress (severe breathing difficulty), and sometimes death.
This article is about the outbreak of SARS that occurred in 2003. For information about the COVID-19 outbreak caused by SARS-CoV-2, please see the Centers for Disease Control and Prevention (CDC) website.
Causes
SARS is caused by the SARS-associated coronavirus (SARS-CoV). It is one of the coronavirus family of viruses (the same family that can cause the common cold). An epidemic of SARS started in 2003 when the virus spread from small mammals to people in China. This outbreak quickly reached global proportions, but was contained in 2003. No new cases of SARS have been reported since 2004.
When someone with SARS coughs or sneezes, infected droplets spray into the air. You can catch the SARS virus if you breathe in or touch these particles. The SARS virus may live on hands, tissues, and other surfaces for up to several hours in these droplets. The virus may be able to live for months or years when the temperature is below freezing.
While the spread of droplets through close contact caused most of the early SARS cases, SARS might also spread by hands and other objects the droplets has touched. Airborne transmission is a real possibility in some cases. Live virus has also been found in the stool of people with SARS, where it has been shown to live for up to 4 days.
With other coronaviruses, becoming infected and then getting sick again (reinfection) is common. This may also be the case with SARS.
Symptoms usually occur 2 to 10 days after coming in contact with the virus. People with active symptoms of illness are contagious. But it is not known for how long a person may be contagious after symptoms appear.
Symptoms
Most people who get SARS will have symptoms.
The main symptoms are:
- Cough
- Difficulty breathing
- Fever of 100.4°F (38.0°C) or higher
- Other breathing symptoms
The most common symptoms are:
- Chills and shaking
- Cough, usually starts 2 to 7 days after other symptoms
- Headache
- Muscle aches
- Tiredness
Less common symptoms include:
- Cough that produces phlegm (sputum)
- Diarrhea
- Dizziness
- Nausea and vomiting
In some people, the lung symptoms get worse during the second week of illness, even after the fever has stopped.
Exams and Tests
Your health care provider may hear abnormal lung sounds while listening to your chest with a stethoscope. In most people with SARS, a chest x-ray or chest CT scan show pneumonia, which is typical with SARS.
Tests used to diagnose SARS might include:
- Arterial blood tests
- Blood clotting tests
- Blood chemistry tests
- Chest x-ray or chest CT scan
- Complete blood count (CBC)
Tests used to quickly identify the virus that causes SARS include:
- Antibody tests for SARS
- Direct isolation of the SARS virus
- Rapid polymerase chain reaction (PCR) test for SARS virus
Treatment
People who are thought to have SARS should be checked right away by a provider. If they are suspected of having SARS, they should be kept isolated in a hospital.
Treatment may include:
- Antibiotics to treat bacteria that cause pneumonia (until bacterial pneumonia is ruled out or if there is bacterial pneumonia in addition to SARS) and to treat bacterial infections that could occur in addition to SARS
- Oxygen, breathing support (mechanical ventilation), or chest therapy
In some serious cases, the liquid part of blood from people who have already recovered from SARS has been given as a treatment.
There is no strong evidence that these treatments work well. There is evidence that the antiviral medicine, ribavirin, does not work. Newer antivirals have not been tried as the disease has not occurred recently.
Outlook (Prognosis)
In the 2003 outbreak, the death rate from SARS was 9% to 12% of those diagnosed. In people over age 65, the death rate was higher than 50%. The illness was milder in younger people.
In the older population, many more people became sick enough to need breathing assistance. And even more people had to be treated in hospital intensive care units.
Public health policies were effective at controlling outbreaks of SARS. Since 2004, there have been no cases of SARS reported anywhere in the world.
Possible Complications
Complications may include:
- Respiratory failure
- Liver failure
- Heart failure
- Kidney problems
When to Contact a Medical Professional
Contact your provider if you or someone you have been in close contact with has SARS.
Prevention
Currently, there is no known SARS transmission anywhere in the world. If a SARS outbreak occurs, reducing your contact with people who have SARS lowers your risk for the disease. Avoid travel to places where there is an uncontrolled SARS outbreak. When possible, avoid direct contact with people who have SARS until at least 10 days after their fever and other symptoms are gone.
- Hand hygiene is the most important part of SARS prevention. Wash your hands or clean them with an alcohol-based instant hand sanitizer.
- Cover your mouth and nose when you sneeze or cough. Droplets that are released when a person sneezes or coughs are infectious.
- DO NOT share food, drink, or utensils.
- Clean commonly touched surfaces with an EPA-approved disinfectant.
Masks and goggles may be useful for preventing the spread of the disease. You may use gloves when handling items that may have touched infected droplets.
References
Gerber SI, Watson JT. PRE-2019 coronaviruses. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 342.
Perlman S, McIntosh K. Coronaviruses, including severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 155.
Review Date: 1/22/2023
Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron Jr. Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.