ERCP
Endoscopic retrograde cholangiopancreatography
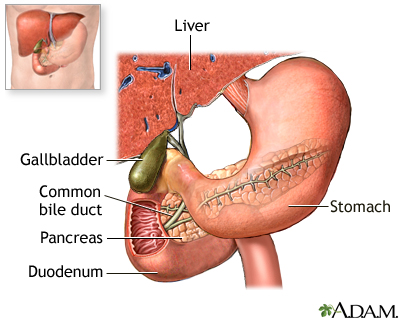
ERCP is short for endoscopic retrograde cholangiopancreatography. It is a procedure that looks at the bile and pancreatic ducts. It is done through an endoscope.
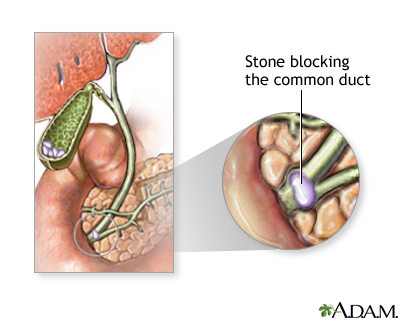
- Bile ducts are the tubes that carry bile from the liver to the gallbladder and small intestine.
- Pancreatic ducts are the tubes that carry fluid from the pancreas into the small intestine.
- ERCP is used to treat and evaluate stones, tumors, or narrowed areas of the bile and pancreatic ducts.
Description
An intravenous (IV) line is placed in your arm. You will lie on your stomach or on your left side for the test.
- Medicines to relax or sedate you will be given through the IV.
- Sometimes, a spray to numb the throat is also used. A mouth guard will be placed in your mouth to protect your teeth. Dentures must be removed.
After the sedative takes effect, the endoscope is inserted through the mouth. It goes through the esophagus (food pipe) and stomach until it reaches the duodenum (the part of the small intestine that is closest to the stomach).
- You should not feel discomfort, and may have little memory of the test.
- You may gag as the tube is passed down your esophagus.
- You may feel stretching of the ducts as the scope is put in place.
A thin tube (catheter) is passed through the endoscope and inserted into the tubes (ducts) that lead to the pancreas and gallbladder. A special dye is injected into these ducts, and x-rays are taken. This helps the doctor see stones, tumors, and any areas that have become narrowed.
Special instruments can be placed through the endoscope and into the ducts.
Why the Procedure Is Performed
The procedure is used mostly to treat or diagnose problems of the pancreas or bile ducts that can cause abdominal pain (most often in the right upper or middle stomach area) and yellowing of the skin and eyes (jaundice).
ERCP may be used to:
- Open the entry of the ducts into the bowel (sphincterotomy)
- Stretch out narrow segments (bile or pancreatic duct strictures)
- Remove or crush gallstones
- Diagnose conditions such as primary biliary cholangitis or sclerosing cholangitis
- Take tissue samples to diagnose a tumor of the pancreas, bile ducts, or gallbladder
- Drain blocked areas
Note: Imaging tests generally will be done to diagnose the cause of symptoms before an ERCP is done. These include ultrasound tests, CT scan, or MRI scan.
Risks
Risks of the procedure include:
- Reaction to the anesthesia, dye, or drug used during the procedure
- Bleeding
- Hole (perforation) of the bowel
- Inflammation of the pancreas (pancreatitis), which can be very serious
Before the Procedure
You will need to not eat or drink for at least 4 hours before the test. You will sign a consent form.
Remove all jewelry so that it will not interfere with the x-ray.
Tell your health care provider if you have allergies to iodine or you have had reactions to other dyes used to take x-rays.
You will need to arrange a ride home after the procedure.
After the Procedure
Someone will need to drive you home from the hospital.
The air that is used to inflate the stomach and bowel during an ERCP procedure can cause some bloating or gas for about 24 hours. After the procedure, you may have a sore throat for the first day. Soreness may last for up to 3 to 4 days.
Do only light activity on the first day after the procedure. Avoid heavy lifting for the first 48 hours.
You can treat pain with acetaminophen (Tylenol). DO NOT take aspirin, ibuprofen, or naproxen. Putting a heating pad on your belly may relieve pain and bloating.
The provider will tell you what to eat. Most often, you will want to drink fluids and eat only a light meal on the day after the procedure.
Contact your provider if you have:
- Abdominal pain or severe bloating
- Bleeding from the rectum or black stools
- Fever above 100°F (37.8°C)
- Nausea or vomiting
References
Cameron J. Gallbladder and biliary tree. In: Cameron J, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:chap 8.
James TW, Baron TH. Endoscopic and radiologic treatment of biliary disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 70.
Lidofsky SD. Jaundice. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 21.
Review Date: 5/3/2023
Reviewed By: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.