Foreign object - inhaled
Obstructed airway; Blocked airway
If you breathe a foreign object into your nose, mouth, or respiratory tract, it may become stuck. This can cause breathing problems or choking. The area around the object also can become inflamed or infected.
Considerations
Children ages 6 months to 3 years are in the age group most likely to breathe in (inhale) a foreign object. These items may include nuts, coins, toys, balloons, or other small items or foods.
Causes
Young children can easily inhale small foods (nuts, seeds, or popcorn) and objects (buttons, beads, or parts of toys) when playing or eating. This may cause a partial or total airway blockage.
Young children have smaller airways than adults. They also can't move enough air when coughing to dislodge an object. Therefore, a foreign object is more likely to get stuck and block the air passage.
Symptoms
Symptoms include:
- Choking
- Coughing
- Difficulty speaking
- No breathing or breathing trouble (respiratory distress)
- Turning blue, red or white in the face
- Wheezing
- Chest, throat or neck pain
Sometimes, only minor symptoms are seen at first. The object may be forgotten until symptoms such as inflammation or infection develop.
First Aid
First aid may be performed on an infant or older child who has inhaled an object. First aid measures include:
- Back blows or chest compressions for infants.
- Abdominal thrusts for older children.
- If the infant or child continues to have trouble breathing, they might need emergency cardiopulmonary resuscitation.
Be sure you are trained to perform these first aid measures.
Parents of infants and young children should consider taking a Basic Life Support class from the American Heart Association.
Any child who may have inhaled an object should be seen by their health care provider. A child with a total airway blockage requires emergency medical help.
If choking or coughing goes away, and the child does not have any other symptoms, he or she should be watched for signs and symptoms of infection or irritation. X-rays may be needed.
A procedure called bronchoscopy may be needed to confirm the diagnosis and to remove the object. Antibiotics and breathing therapy may be needed if an infection develops.
Do Not
Do not force feed infants who are crying or breathing rapidly. This may cause the baby to inhale liquid or solid food into their airway.
When to Contact a Medical Professional
Contact your provider or call 911 or the local emergency number if you think a child has inhaled a foreign object.
Prevention
Preventive measures include:
- Keep small objects out of the reach of young children.
- Discourage talking, laughing, or playing while food is in the mouth.
- Do not give potentially dangerous foods such as hot dogs, whole grapes, nuts, popcorn, food with bones, or hard candy to children under age 3.
- Teach children to avoid placing foreign objects into their noses and other body openings.
References
Gorelik M, Schroeder JW. Foreign bodies in the airway. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 435.
Hairston TK, McNamara L. Emergency and critical care management. In: Kleinman K, Mcdaniel L, Molloy M, eds. Harriet Lane Handbook, The. 23rd ed. Philadelphia, PA: Elsevier; 2024:chap 1.
Marcdante KJ, Kliegman RM, Schuh AM. Upper airway obstruction. In: Marcdante KJ, Kliegman RM, Schuh AM, eds. Nelson Essentials of Pediatrics. 9th ed. Elsevier; 2023:chap 135.
Shah SR, Little DC. Ingestion of foreign bodies. In: Holcomb GW, Murphy JP, St. Peter SD, eds. Holcomb and Ashcraft's Pediatric Surgery. 7th ed. Philadelphia, PA: Elsevier; 2020:chap 11.
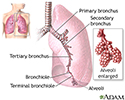
Lungs - illustration
Lungs
illustration
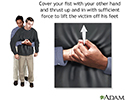
Heimlich maneuver on adult - illustration
Heimlich maneuver on adult
illustration
Heimlich maneuver on an adult - illustration
Heimlich maneuver on an adult
illustration
Heimlich maneuver on oneself - illustration
Heimlich maneuver on oneself
illustration
Heimlich maneuver on infant - illustration
Heimlich maneuver on infant
illustration
Heimlich maneuver on infant - illustration
Heimlich maneuver on infant
illustration
Heimlich maneuver on conscious child - illustration
Heimlich maneuver on conscious child
illustration
Heimlich maneuver on conscious child - illustration
Heimlich maneuver on conscious child
illustration
Lungs - illustration
Lungs
illustration
Heimlich maneuver on adult - illustration
Heimlich maneuver on adult
illustration
Heimlich maneuver on an adult - illustration
Heimlich maneuver on an adult
illustration
Heimlich maneuver on oneself - illustration
Heimlich maneuver on oneself
illustration
Heimlich maneuver on infant - illustration
Heimlich maneuver on infant
illustration
Heimlich maneuver on infant - illustration
Heimlich maneuver on infant
illustration
Heimlich maneuver on conscious child - illustration
Heimlich maneuver on conscious child
illustration
Heimlich maneuver on conscious child - illustration
Heimlich maneuver on conscious child
illustration
Review Date: 4/9/2024
Reviewed By: Frank D. Brodkey, MD, FCCM, Associate Professor, Section of Pulmonary and Critical Care Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.