Placenta abruptio
Premature placental separation; Placental separation; Placental abruption; Vaginal bleeding - abruption; Pregnancy - abruption
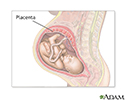
The placenta connects the fetus (unborn baby) to the mother's uterus. It allows the baby to get nutrients, blood, and oxygen from the mother. It also helps the baby get rid of waste.
Placenta abruptio (also called placental abruption) is when the placenta separates from the inner wall of the uterus before the baby is born.
More About This Condition
In most pregnancies, the placenta stays attached to the upper part of the uterine wall.
In a small number of pregnancies, the placenta detaches (pulls itself from the wall of the uterus) too early. Most of the time, only part of the placenta pulls away. Other times it pulls away completely. If this happens, it is most often in the 3rd trimester.
The placenta is the lifeline of a fetus. Serious problems occur if it detaches. The baby gets less oxygen and fewer nutrients. Some babies become growth restricted (very small), and in a small number of cases, it is fatal. It can also cause significant blood loss for the mother.
What Causes It?
No one knows what causes placental abruption. But these factors raise a woman's risk for it:
- History of placental abruption in previous pregnancy
- Long-term (chronic) high blood pressure
- Presence of preeclampsia
- Sudden high blood pressure in pregnant women who had normal blood pressure in the past
- Heart disease
- Abdominal trauma
- Smoking
- Alcohol or cocaine use
- Fibroids in the uterus
- An injury to the mother (such as a car crash or fall in which the abdomen was hit)
- Being older than 40
- Medical conditions with increased risks of blood clotting
Signs of Placental Abruption
The most common symptoms are vaginal bleeding and painful contractions. The amount of bleeding depends on how much of the placenta has detached. Sometimes the blood that collects when the placenta detaches stays between the placenta and uterine wall, so you may not have bleeding from your vagina.
- If the separation is slight, you may have only light bleeding. You may also have cramps or feel tender in your belly.
- If the separation is moderate, you may have heavier bleeding. Cramps and belly pain will be more severe.
- If more than half the placenta detaches, you may have belly pain and heavy bleeding. You may also have contractions. The baby may move more or less than normal.
If you have any of these symptoms during your pregnancy, tell your health care provider right away.
How is Placental Abruption Treated?
Your provider will:
- Do a physical exam
- Observe your contractions and how your baby responds to them
- Sometimes do an ultrasound to check your placenta (but ultrasound does not always show a placental abruption)
- Check your baby's heart rate and rhythm
If your placental abruption is small, your provider may put you on bed rest to stop your bleeding. After a few days, most women can go back to their normal activities in most cases.
For a moderate separation, you will likely need to stay in the hospital. In the hospital:
- Your baby's heart rate will be monitored.
- You might need a blood transfusion.
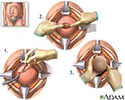
- If your baby shows any signs of distress, your provider may induce your labor early. If you cannot give birth vaginally, you will need a C-section.
Severe placental abruption is an emergency. You will need to deliver right away, most often by C-section. It is very rare, but a baby can be stillborn if there is a severe abruption.
Can I Prevent Placental Abruption?
You cannot prevent placental abruption, but you can control the risk factors related to it by:
- Keeping high blood pressure, heart disease, and diabetes under control
- Not using tobacco, alcohol, or cocaine
- Following your provider's recommendations about ways to lower your risk if you had an abruption in a past pregnancy
References
Francois KE, Foley MR. Antepartum and postpartum hemorrhage. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Henn MC, Lall MD. Complications of pregnancy. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 173.
Hull AD, Resnik R, Silver RM. Placenta previa and accreta, vasa previa, subchorionic hemorrhage, and abruptio placentae. In: Lockwood CJ, Copel JA, Dugoff L, et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2023:chap 43.
Cesarean section - illustration
Cesarean section
illustration
Ultrasound in pregnancy - illustration
Ultrasound in pregnancy
illustration
Anatomy of a normal placenta - illustration
Anatomy of a normal placenta
illustration
Placenta - illustration
Placenta
illustration
Placenta - illustration
Placenta
illustration
Ultrasound, normal placenta - Braxton Hicks - illustration
Ultrasound, normal placenta - Braxton Hicks
illustration
Ultrasound, normal fetus - arms and legs - illustration
Ultrasound, normal fetus - arms and legs
illustration
Ultrasound, normal relaxed placenta - illustration
Ultrasound, normal relaxed placenta
illustration
Ultrasound, color - normal umbilical cord - illustration
Ultrasound, color - normal umbilical cord
illustration
Placenta - illustration
Placenta
illustration
Cesarean section - illustration
Cesarean section
illustration
Ultrasound in pregnancy - illustration
Ultrasound in pregnancy
illustration
Anatomy of a normal placenta - illustration
Anatomy of a normal placenta
illustration
Placenta - illustration
Placenta
illustration
Placenta - illustration
Placenta
illustration
Ultrasound, normal placenta - Braxton Hicks - illustration
Ultrasound, normal placenta - Braxton Hicks
illustration
Ultrasound, normal fetus - arms and legs - illustration
Ultrasound, normal fetus - arms and legs
illustration
Ultrasound, normal relaxed placenta - illustration
Ultrasound, normal relaxed placenta
illustration
Ultrasound, color - normal umbilical cord - illustration
Ultrasound, color - normal umbilical cord
illustration
Placenta - illustration
Placenta
illustration
Review Date: 11/21/2022
Reviewed By: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.