Infertility in women - InDepth
Pelvic inflammatory disease - InDepth; Polycystic ovary syndrome - InDepth; Inability to conceive - InDepth; Unable to get pregnant - InDepth
An in-depth report on the causes, diagnosis, treatment, and prevention of female infertility.
Highlights
Risk Factors
Risk factors for female infertility include:
Age.
Fertility begins to decline when a woman reaches her mid-30s, and rapidly declines after her late 30s.Weight.
Extreme weight levels, either high or low, can contribute to infertility.Smoking.
Cigarette smoking can impair a woman's fertility.Alcohol.
More than 2 drinks a day may impair a woman's fertility.
Causes
Female infertility may be caused by an underlying medical condition that damages the fallopian tubes, interferes with ovulation, or causes hormonal complications. These medical conditions include:
- Pelvic inflammatory disease
- Endometriosis
- Polycystic ovary syndrome
- Premature ovarian failure
- Thyroid or other hormonal problems
Infertility may also be due to an infertile male partner.
Diagnosis
For women under the age of 35, if you have been unable to conceive after 1 year of unprotected sex, talk with your health care provider about having your fertility evaluated. If you are age 35 or older, you should talk to a fertility specialist if you do not conceive within six months of unprotected sex. Fertility testing should especially be performed if a woman is over 35 years old or if either partner has known risk factors for infertility. An analysis of the man's semen should be performed before the female partner undergoes any invasive testing.
Treatment
Treatment for infertility should first address any underlying medical condition that may be contributing to fertility problems. If this step does not restore fertility, there are several treatment approaches:
- Lifestyle measures (such as maintaining a healthy weight, quitting smoking, limiting alcohol consumption, timing sexual activity with regard to the ovulation cycle)
- Drugs to induce ovulation, such as clomiphene or gonadotrophins
- Surgery to correct blocked fallopian tubes or other structural problems
- Assisted reproductive technologies (ART), such as in vitro fertilization (IVF)
Lifestyle Tips for Optimizing Natural Fertility
The American Society for Reproductive Medicine (ASRM) has guidelines for how couples can increase the likelihood of achieving pregnancy (these recommendations apply to couples who have no evidence of infertility):
- For women who have regular menstrual cycles, having sexual intercourse every other day during the "fertile window" can increase the chances for conception. The fertile window is the 6 days leading up to and including ovulation.
- Couples should avoid using water-based sexual lubricants because they can damage the sperm's ability to swim. Instead, try mineral oil, canola oil, or commercial "fertility friendly" labeled products.
- There is no evidence that certain sexual positions, or resting after sex, boost fertility or increase the odds for getting pregnant.
Introduction
Infertility is the failure of a couple to become pregnant after 1 year of regular, unprotected sexual intercourse. In most cases, infertility is actually decreased fertility due to a number of treatable conditions and not genuine sterility, which is a rare.
About a third of infertility problems are due to female infertility, and another third are due to male infertility. In the remaining cases, infertility affects both partners or the cause is unclear.
Female infertility may occur when:
- The ovaries have problems producing eggs
- An egg cannot move from the ovary to the womb through the fallopian tube
- The fertilized egg does not attach to the lining of the uterus
- A fertilized egg or embryo does not survive once it attaches to the lining of the uterus
The Female Reproductive System
In order to understand infertility, it is important to know the organs and structures of the female reproductive system:
- The
uterus
(womb) is a pear-shaped organ located between the bladder and rectum. It consists of two parts, the body and the cervix. The main function of the uterus is to support the developing fetus. - The
cervix
is the lower part of the uterus. The cervix contains the cervical canal, which connects the uterus to thevagina
. The opening of the cervix, called theos
, is at the top of the vagina. - The
ovaries
are two almond-shaped organs located on either side of the uterus. Ovaries produce hormones and eggs (ova). Ovaries contain thousands of fluid-filled sacs calledfollicles
. Each ovarian follicle houses an immature egg. A dominant follicle produces a mature egg, which is released at the time of ovulation. - Each ovary is attached to a
fallopian tube
, which connects to the upper part of the uterus. When an egg is released by an ovary, it travels to the fallopian tube to await fertilization. - If fertilization occurs, the egg moves to the uterus and implants in the lining. If no fertilization occurs, the egg moves to the uterus and disintegrates.
The uterus is a hollow muscular organ located in the female pelvis between the bladder and rectum. The ovaries produce the eggs that travel through the fallopian tubes. Once the egg has left the ovary it can be fertilized and implant itself in the lining of the uterus.
The Reproductive Cycle
During a woman's monthly menstrual cycle, her body prepares for conception and pregnancy. The average menstrual cycle is about 28 days but a normal cycle can range from 21 to 35 days. The menstrual cycle is divided into three phases: follicular, ovulatory, and luteal.
Follicular Phase (Days 1 to 13)
The follicular phase begins with the first day of menstrual bleeding:
- Estrogen and progesterone hormones are at their lowest levels. This causes the uterine lining (endometrium) to break down and shed.
- The hypothalamus in the brain produces gonadotropin-releasing hormone (GnRH), which stimulates the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH and LH trigger the production of estrogen.
- As FSH levels increase, they stimulate the growth and maturation of eggs in the ovarian follicles. About 15 to 20 follicles are stimulated, but only 1 follicle continues to mature.
- The dominant follicle produces estrogen. The other follicles stop growing and disintegrate.
Ovulatory Phase (Day 14)
The ovulatory phase occurs halfway through the menstrual cycle. During the ovulatory phase:
- The increase in estrogen from the dominant follicle triggers a surge in LH. As estrogen levels rise, they prompt the cervix to secrete more mucus to help nourish and propel sperm to the egg.
- The LH surge signals the dominant follicle to burst and release the developed egg into the fallopian tube. The release of the egg is called ovulation. Once in the fallopian tube, the egg is in place for fertilization.
- The egg can live for 12 to 24 hours after being released. Sperm can live for up to 7 days in a women's body.
- A woman's fertile window, when she is most likely to get pregnant, is about 6 days long. It starts 5 days before ovulation and ends the day of ovulation.
Luteal Phase (Days 15 to 28)
The luteal phase begins immediately after ovulation and ends when the next menstrual period starts. The luteal phase lasts about 12 to 16 days. During the luteal phase:
- After releasing the egg, the ruptured follicle closes and forms
corpus luteum
, a yellow mass of cells that provide a source of estrogen and progesterone during pregnancy. These hormones help the uterine lining to thicken and prepare for the egg's implantation. - If the egg is fertilized by a sperm cell, it implants in the lining of the uterus and pregnancy begins.
- If fertilization does not occur, the egg breaks apart. The corpus luteum degenerates, and estrogen and progesterone levels drop. The thickened uterine lining sloughs off and is shed along with the unfertilized egg during menstruation. The menstrual cycle begins again.
Fertilization and Pregnancy
Conception occurs when an egg is fertilized by a sperm. When fertilization occurs:
- The fertilized egg (zygote) immediately begins to divide until it becomes a ball of cells known as a blastocyst.
- The blastocyst moves from the fallopian tube into the uterus where it is implanted in the uterine lining. Implantation takes place about 6 to 10 days after fertilization. Implantation is when pregnancy begins.
- The inner cells of the blastocyst become the embryo, which develops into the fetus. The outer cells of the blastocyst become the placenta. The placenta is a thick blanket of blood vessels that nourishes the fetus as it develops.
- The placenta produces and secretes the hormone human chorionic gonadotropin (hCG), which helps signal the corpus luteum (the yellow tissue formed from the ruptured follicle) to continue to produce estrogen and progesterone. After about 10 weeks, the placenta takes over production of progesterone and estrogen, and the corpus luteum degenerates.
Causes
Most cases of female infertility are due to medical conditions that cause:
- Ovulation problems
- Blocked fallopian tubes
- Structural problems in the reproductive system
- Problems with quality of cervical mucus or eggs
Ovulation Problems
Ovulation is the release of the egg that occurs during the monthly menstrual cycle. Problems that affect ovulation, and the hormones involved with ovulation, are the most common cause of female infertility. These conditions include:
Polycystic Ovarian Syndrome (PCOS).
In PCOS, the ovaries produce excessive amounts of androgens (male hormones), particularly testosterone. Increased androgen production results in high levels of LH and low levels of FSH, so that follicles are prevented from producing a mature egg. The development of follicles is stopped short of releasing of the egg. This arrested development of the follicles leads to ovaries that have many small, immature follicles that have never released an egg. On ultrasound exam, these multiple follicles are easily seen as small cysts or fluid collections. Women with PCOS do not ovulate regularly and they experience infrequent or absent menstrual cycles.
Premature Ovarian Failure.
Premature ovarian failure, also called primary ovarian insufficiency, is when ovaries stop functioning normally before age 40. It is often caused by hormonal or genetic issues, which deplete the follicles. This condition is not the same as premature menopause (cessation of menstrual periods). Women with primary ovarian failure may still have occasional periods.Elevated Prolactin Levels.
Prolactin is a hormone produced in the pituitary gland that stimulates breast development and milk production in association with pregnancy. High levels of prolactin (hyperprolactinemia) reduce gonadotropin hormones and inhibit ovulation. Hyperprolactinemia in women who are not pregnant or nursing can be caused by an underactive thyroid gland, pituitary gland problems, or certain types of medications.
Blocked Fallopian Tubes
A blocked fallopian tube can prevent sperm from reaching and fertilizing the egg. Blockage in the fallopian tubes can also prevent a fertilized egg from traveling to the uterus for implantation. Conditions that can block or damage fallopian tubes include:
Pelvic Inflammatory Disease (PID).
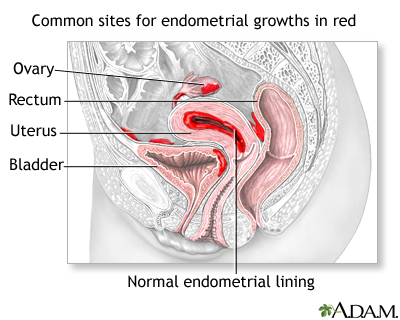
PID refers to infection in the pelvic area and reproductive tract, including the fallopian tubes. PID is a complication of bacterial infection. The most common causes are sexually transmitted infections, such as chlamydia and gonorrhea. In addition to infertility, history of PID can increase the risk for ectopic pregnancy, where the embryo implants in the fallopian tube or another location outside of the uterus.Endometriosis.
Endometriosis is a condition in which cells that line the uterus grow in areas outside of the uterus. Endometrial implants in the fallopian tubes may block the egg's passage, while implants that occur in the ovaries can prevent the release of the egg. Severe endometriosis can form bands of scar tissue (adhesions) between the uterus, ovaries, and fallopian tubes that prevent egg transfer. Endometriosis frequently causes chronic inflammation of the pelvic organs, this inflammation may reduce the chance of becoming pregnant.
Endometriosis is a noncancerous condition in which cells that normally line the uterus (endometrium) also grow on other areas of the body, causing pain and abnormal bleeding.
Scarring.
Adhesions (scar tissue) can be caused by conditions besides endometriosis. Adhesions that form after abdominal or pelvic surgery or infection can block ovaries and fallopian tubes and cause infertility.
Structural Problems
Structural problems in a women's reproductive system may be caused by:
Congenital Conditions.
Sometimes women are born with reproductive tract abnormalities that may cause infertility. These malformations typically affect the uterus or vagina. For example, daughters born to women who took the drug diethylstilbestrol (DES) during pregnancy are at increased risk of having uterine structural abnormalities associated with infertility.Uterine Fibroids.
Uterine fibroids are non-cancerous growths that originate in the walls of the uterus. They may contribute to infertility by distorting the shape of the uterine cavity. Fibroids may also impair blood flow to the uterine lining.Adenomyosis.
Adenomyosis is a thickening of the uterus. It occurs when endometrial tissue, which normally lines the uterus, moves into the outer walls of the uterus. During IVF, adenomyosis may reduce the chance of implantation or may lead to early pregnancy loss.
Cervical Mucus and Egg Quality
Cervical Mucus
Low amounts of cervical mucus or poor quality cervical mucus can contribute to infertility by interfering with the sperm's ability to reach and fertilize the egg.
Ovarian Reserve
Ovarian reserve refers to the quality and quantity of a woman's eggs. As a woman ages, the number and quality of her eggs diminish. Younger women can also have problems with ovarian reserve, usually because of medical conditions or treatments that affect the ovaries.
Other Causes of Infertility
Hypothyroidism (underactive thyroid gland) and type 1 diabetes are some of the medical conditions that can contribute to infertility. Other autoimmune diseases such as multiple sclerosis and rheumatoid arthritis can affect fertility.
Risk Factors
Age
Fertility declines as a woman ages. Fertility begins to decrease when a woman reaches age 32, and rapidly declines after age 37. As a woman ages, her ovaries produce fewer eggs. In addition, the quality of the eggs is poorer than those of younger women. Older women also have a higher risk of miscarriage. Older women are also more likely to have health problems that may interfere with fertility.
Weight
Although most of a woman's estrogen is manufactured in her ovaries, smaller amounts are produced by fat cells, which transform male hormones produced by the adrenal glands into estrogen. Because a normal hormonal balance is essential for the process of conception, extreme weight levels (either high or low) can contribute to infertility.
Being Overweight
Being overweight or obese can contribute to infertility in various ways. Obesity is also associated with PCOS, an endocrine disorder that can cause infertility.
Being Underweight
Being extremely underweight is a risk factor for infertility. Body fat levels that are significantly below normal can completely shut down the ovulation process.
Smoking
Cigarette smoking can harm a woman's ovaries and contribute to a decrease in eggs. The cells that line the fallopian tubes may also slow down their ability to move the fertilized egg into the uterine cavity for implantation, resulting in abnormal pregnancies. Smoking may also interfere with the success of fertility treatments.
Alcohol and Caffeine Use
Alcohol and caffeine use may contribute to infertility. If you are trying to become pregnant, it is best to avoid alcohol. Alcohol use in early pregnancy can contribute to birth defects. Moderate coffee intake does not increase the risk for infertility and does not decrease the success rate of IVF. However, try to limit consumption to no more than 2 cups of coffee a day. Drinking more than 5 cups of coffee a day may reduce fertility.
Environmental Factors
Exposure to environmental hazards (such as herbicides, pesticides, and industrial solvents) may affect fertility. Estrogen-like chemicals that interfere with normal hormones are of particular concern for infertility in men and for effects on offspring of women. Phthalates, chemicals used to soften plastics, are under particular scrutiny because they may disrupt hormones.
Stress
Neurotransmitters (chemical messengers in the brain) act in the hypothalamus gland, which controls both reproductive and stress hormones. There is no conclusive evidence that stress has any significant effect on fertility or fertility treatments.
Diagnosis
Both male and female partners should get tested for infertility if pregnancy fails to occur after 1 year of regular unprotected sexual intercourse. If a woman is over age 35, fertility testing is recommended if she fails to conceive after 6 months of unprotected sex
Most couples who do not have fertility problems conceive within the first 6 months of attempting pregnancy, and typically within the first 3 months.
An analysis of the man's semen should be performed before the female partner undergoes any invasive testing.
Ovulation Home Tests
Before beginning an expensive fertility work-up, you can try the following steps at home. They are free or low-cost and may be helpful:
Monitor basal body temperature.
Basal body temperature (BBT) is the body's lowest natural temperature at rest. Because BBT increases slightly during ovulation, tracking and charting your BBT may help you determine when ovulation takes place. You can monitor your BBT by taking your temperature at the same time every morning using a regular thermometer or a special digital BBT thermometer that stores and displays the data.Test the consistency of your cervical mucus.
Collect some mucus between two fingers and stretch it apart. If you are near the time of ovulation, the mucus will stretch more than 1 inch before it breaks.Use an over-the-counter urine test to detect luteinizing hormone (LH) surges.
This helps determine the day of ovulation. Tests are also available to measure levels of FSH. However, these at-home tests may not be as accurate as those performed in a medical office.
Medical History and Physical Examination
The first step in any infertility work-up is a complete medical history and physical examination. Your provider will ask about:
- Health conditions that may contribute to infertility (endometriosis, sexually transmitted infections, thyroid disorders, PCOS)
- Menstrual history (when you first began menstruating, the frequency and regularity of your periods)
- Reproductive history (prior pregnancies or miscarriages)
- Sexual history (how often you have sex, how long you have been trying to get pregnant)
- Lifestyle issues (smoking, drug and alcohol use)
The provider may feel your thyroid gland to check for signs of nodules or enlargement. A pelvic exam will evaluate any signs of masses or structural abnormalities.
Laboratory Tests
Hormone Levels
Various tests are used to evaluate hormone function and ovarian reserve (the number of follicles and quality of the eggs). These include blood tests for FSH, antimullerian hormone (AMH), progesterone, and estradiol, and urine tests for LH. You may also receive tests to check your thyroid hormone and prolactin levels. Blood tests for previous infections with chlamydia may also be considered and can help women avoid more invasive procedures like laparoscopy.
Clomiphene Challenge Test
Clomiphene citrate (Clomid, Serophene, generic), a standard fertility drug, may be used to test for ovarian reserve. With this test, blood is drawn to measure FSH on day 3 of the menstrual cycle. The woman takes clomiphene on days 5 to 9 of the cycle. FSH is tested again on day 10. A normal response to clomiphene is a moderate increase in FSH levels followed by a return to baseline. High levels of FSH on day 3 or day 10 indicate problems with ovarian function. However, a normal result of the clomiphene test does not necessarily guarantee a good response to fertility treatments.
Imaging Tests
Imaging tests are used to examine the uterus and fallopian tubes.
Ultrasound and Sonohysterography
Ultrasound is the standard imaging technique for evaluating the uterus and ovaries. It uses a probe placed in the vagina to send out sound waves, which produce an image of the organs. Transvaginal sonohysterography uses ultrasound along with saline infused into the uterus. This helps enhance the image and improve the detection of potential problems.
Hysterosalpingography
Hysterosalpingography is an x-ray procedure performed to discover possible blockage in the fallopian tubes and abnormalities in the uterus:
- The provider inserts a tube into the cervix through which a special dye is injected.
- The dye passes into the uterus and up through the fallopian tubes.
- An x-ray is taken of the dye-filled uterus and tubes.
- If the dye is seen emerging from the end of the tube, no blockage is present. (In some cases, hysterosalpingography may even restore fertility by clearing away tiny tubal blockages.)
- If results show blockage or abnormalities, the test may need to be repeated. In case of blockage, hysterosalpingography may reveal conditions, such as endometrial polyps, uterine fibroids, or structural abnormalities of the uterus and tubes.
Surgical Diagnostic Procedures
Hysteroscopy
Hysteroscopy uses a long flexible or rigid tube called a hysteroscope, which is inserted into the vagina and advanced through the cervix to reach the uterus. A fiber-optic light source and a tiny camera in the tube allow the doctor to view the uterus, ovaries, and fallopian tubes.
Hysteroscopy may be done in a medical office or in a hospital operating room, depending on whether local or general anesthesia is used. The uterus is filled with saline or carbon dioxide to inflate the cavity and provide better viewing. This can cause cramping.
Laparoscopy
Laparoscopy is a minimally invasive surgical procedure. It requires general anesthesia and is performed in an operating room. The surgeon makes a very small incision below the belly button and inserts an instrument called a laparoscope, which is similar to a hysteroscope. (The difference is that a laparoscope is inserted through the abdomen, while a hysteroscope is inserted through the vagina and cervix.)
Through the laparoscope, the surgeon can view the uterus, fallopian tube, and ovaries. Laparoscopy is most helpful for identifying endometriosis or other adhesions that may affect fertility.
Treatment
Fertility Treatment Approaches
Several approaches are used to treat infertility:
- Drugs to induce ovulation, such as clomiphene and gonadotrophins
- Surgery to correct blockage in the fallopian tubes or other structural problems, such as fibroids
- Assisted reproductive technologies (ART) such as IVF
- Lifestyle measures are also important. They include maintaining a healthy weight, quitting smoking, and timing sexual activity with ovulation cycle.
Choosing a Fertility Clinic
Advanced fertility procedures and medications are expensive and often not covered by insurance. Choosing a good fertility clinic is important. You should ask the fertility clinic questions about:
- The live-birth success rate, not just pregnancy success rate. (Multiple births, such as twins or triplets, are counted as one live birth.)
- How many cycles of treatment the clinic performs each year.
- The qualifications and training of the fertility specialists.
- What treatments are available.
- How your age may affect the choice of treatment.
- Whether your treatments will be covered by insurance.
Special Considerations for Women with Cancer
Women undergoing cancer treatments who are concerned about preserving their fertility should see a reproductive specialist to discuss their options These discussions should take place as early as possible, and before cancer treatment starts.
According to the American Society of Clinical Oncology's guidelines, the best fertility preservation methods for women with cancer are embryo and oocyte (egg) cryopreservation. This procedure involves harvesting and freezing a woman's eggs (oocytes), and can be followed by IVF and freezing of embryos for later use. It requires several weeks of pretreatment with ovarian stimulation drugs, so planning is very important.
Ovarian transposition, which involves moving one or both ovaries outside of the treatment field, may be an option for some women who are undergoing pelvic radiation. If you are going to be having gynecological surgery or radiation as part of your cancer treatment, discuss with your cancer care team any options for procedures that may help conserve fertility. And, be sure your doctors clearly explain to you how various cancer treatments could affect your fertility.
Embryo and oocyte cryopreservation are well-established methods that have excellent chances for success. At this time, other fertility preservation methods such as ovarian tissue cryopreservation, are still considered experimental and the American Society of Clinical Oncology does not recommend them.
Treatment of Fibroids
Fibroids originate from the thick wall of the uterus and are categorized by where they grow. Treatment recommendations are based on the size and type of the fibroid.
Intramural fibroids.
Grow within the middle and thickest layer of the uterus. Surgical removal of these fibroids (myomectomy) is generally not recommended as a treatment for unexplained infertility.Subserosal fibroids.
Grow out from the thin outer fibrous layer of the uterus (called the serosa). Removal of this type of fibroid is not recommended in the treatment of infertility.Submucosal fibroids.
Grow from the uterine wall toward and into the inner lining of the uterus (the endometrium). Removal of this type of fibroid is recommended in women whose infertility is otherwise not explained. It can be done using a hysteroscope if they are less than 5 cm in size.
Uterine artery embolization is a less invasive treatment for fibroids. This procedure blocks blood supply to a fibroid, causing it to shrink. However, this treatment is generally not recommended for women seeking future pregnancies.
Medications
Medications to treat infertility can be divided into three main categories:
Medications for Ovarian Stimulation.
These drugs are often used alone as initial treatment to induce ovulation, particularly for women who have medical conditions that cause ovulation problems. They may also be used along with ART to stimulate multiple eggs to grow in the ovaries, a process called superovulation. The main drugs used for ovarian stimulation are clomiphene, FSH, LH, and human menopausal gonadotrophin (hMG, also called menotropin, which is a combination of FSH and LH).Medications for Oocyte Maturation.
Drugs such as hCG are used during ART to help the ovarian follicles ripen (mature)Medications to Prevent Premature Ovulation.
These drugs are used during ART to help prevent premature ovulation. They include GnRH agonists and GnRH antagonists.
Other drugs may also be used, for example:
Letrazole (Femara)
is an aromatase inhibitor that is not approved for treatment of infertility but is often used "off-label" for ovarian stimulation. It is often used as a first-line fertility treatment for women with PCOS. However, for unexplained infertility, it is not as helpful as more standard drugs.Metformin
is a common drug used to treat type II diabetes. For women with PCOS, metformin may help reduce the chance of ovarian hyperstimulation.
Clomiphene
Clomiphene citrate (Clomid, Serophene, generic) is usually the first fertility drug prescribed for women who have ovulation problems. (It is less likely to work for women who have normal ovulation.)
Unlike more potent drugs used in superovulation, clomiphene is gentler and works by blocking estrogen, which tricks the pituitary into producing the hormones FSH and LH. This process boosts follicle growth and the release of the egg.
Clomiphene can be taken by mouth, is relatively inexpensive, and the risk for multiple births is lower than with other drugs. One or two tablets are taken each day for 5 days, usually starting 2 to 5 days after the period starts. If successful, ovulation occurs about a week after the last pill has been taken. If ovulation does not occur, then a higher dose may be given for the next cycle.
If this regimen is not successful, treatment may be repeated or additional drugs may be added. Health care providers usually do not recommend more than 6 cycles.
Mood swings are a very common side effect of clomiphene. Other side effects include hot flashes, breast tenderness, nausea, pelvic discomfort, and ovarian cysts.
Gonadotropins
If clomiphene does not work or is not an appropriate choice, gonadotropin drugs are a second option. Gonadotropins include several different types of drugs that contain either a combination of the hormones FSH and LH, or only FSH.
Whereas clomiphene works indirectly by stimulating the pituitary gland to secrete FSH, which prompts follicle production, gonadotropin hormones directly stimulate the ovaries to produce multiple follicles.
Gonadotropins are given by injection. Your doctor may show you how to self-administer the injection. Gonadotropins include:
- Human menopausal gonadotropins (hMG), also called menotropin, is a combination of FSH with LH
- Human chorionic gonadotropins (hCG)
- Follicle stimulating hormone (FSH)
- Gonadotropin-releasing hormone (GnRH) analogs, which include GnRH agonists and GnRH antagonists
Human Menopausal Gonadotropin (hMG)
The hMG drugs contain a mixture of both FSH and LH. These drugs (Menopur, Repronex, and Humegon) are all derived from the urine of postmenopausal women. hMG is administered as a series of injections 2 to 3 days after the period starts. Injections are usually given for 7 to 12 days, but the time may be extended if ovulation does not occur. In such cases, a shot of hCG may trigger ovulation.
Human Chorionic Gonadotropin (hCG)
The hCG drugs are similar to LH. It mimics the LH surge, which stimulates the follicle to release the egg. Natural hCG drugs, derived from the urine of pregnant women, include Pregnyl, Profasi, and Novarel. Ovidrel is a genetically modified hCG drug. Ovidrel has fewer side effects and its quality can be better controlled than the natural drugs. It is generally used after hMG or FSH to stimulate the final maturation stages of the follicles. Ovulation, if it occurs, does so about 36 to 72 hours after administration.
Follicle Stimulating Hormone (FSH)
Urofollitropin (Bravelle, Fertinex) is a purified form of FSH, derived from the urine of postmenopausal women. Follitropin drugs (Gonal-F, Follistim) are synthetic versions of FSH. These FSH drugs are sometimes given in combination with an hCG drug.
GnRH Analogs (Agonists or Antagonists)
Gonadotropin-releasing hormone (GnRH) is a hormone produced in the hypothalamus part of the brain. GnRH stimulates the pituitary gland to produce LH and FSH.
GnRH analogs are synthetic forms of GnRH. They are similar to natural GnRH but have very different actions. These drugs actually prevent the LH and FSH surge that occurs right before ovulation. This action helps prevent the premature release of the eggs before they can be harvested for ART.
GnRH analogs are classified as either agonists or antagonists:
- GnRH agonists include leuprolide (Lupron, Eligard, generic), nafarelin (Synarel), and goserelin (Zoladex)
- GnRH antagonists include ganarelix (Antagon) and cetrorelix (Cetrotide)
Risks for Superovulation
Superovulation is the process of using fertility drugs to stimulate the development of multiple follicles (eggs) in the ovaries. Superovulation is also calledcontrolled ovarian stimulation
.Potential risks and complications of superovulation include:
Multiple Births.
Superovulation increases the risks for multiple births. The risk is highest for twins. The exact risks depend in part on the drug used and whether it is used along with ART.Ovarian Hyperstimulation Syndrome (OHSS).
The most serious risk of superovulation is OHSS, a condition in which the ovaries become enlarged and filled with fluid. In severe cases, this can lead to life-threatening complications including blood clots, liver and kidney damage, and dangerous fluid and electrolyte imbalances. Symptoms include abdominal bloating and pain, weight gain, nausea and vomiting, and shortness of breath.Cancer Concerns.
There has been concern that clomiphene and gonadotropins may increase the risks for ovarian and breast cancer. Most evidence to date does not indicate that ovulation-stimulating drugs increase the risks for these types of cancers.
Assisted Reproductive Technologies (ART)
ART are medical techniques that help couples conceive. These procedures involve either:
- A couple's own eggs or sperm
- Donor eggs, sperm, or embryos
Fertilization may occur either in the laboratory or in the uterus. In the United States, over 68,000 live births (deliveries of one or more infants) occur each year using ART. According to the Centers for Disease Control (CDC), approximately 1.7% of all babies born in the United States every year are conceived using ART.
Technically, the term ART refers only to fertility treatments, such as IVF and its variants, which handle both egg and sperm.
Intrauterine Insemination (IUI)
Artificial insemination (AI) involves placing the sperm directly in the cervix (called intracervical insemination) or into the uterus (called intrauterine insemination, or IUI).
IUI is the standard AI procedure. It involves placing washed sperm into the woman's uterine cavity through a long, thin catheter. The washing procedure produces high quality sperm by removing seminal fluid and non-motile (not moving) cells, infectious agents, and chemicals used in the cryopreservation of semen. The sperm can come from the woman's male partner or from a donor (third party). The procedure is usually performed for cases of male infertility or unexplained female infertility. It may also be used if a woman has cervical scarring that prevents sperm from entering the uterus.
An IUI procedure is performed close to the time of ovulation. If a woman ovulates naturally, she may have ultrasound or other imaging tests performed to monitor for signs of ovulation. She may also use an ovarian prediction kit at home to test for the LH surge that occurs a few days before ovulation.
IUI is also frequently performed in combination with fertility drugs in a process called controlled ovarian stimulation. These drugs include clomiphene and letrozole, which may be used along with an injection of hCG. The sperm is inserted 1 to 2 days after the hCG injection.
You will take a pregnancy test a few weeks after the procedure. If pregnancy was not achieved, the cycle may be repeated.
IUI is the least complex and least expensive of fertility procedures and is often tried first in uncomplicated cases of infertility. However, it may pose a greater risk for multiple births and have a lower chance for pregnancy success than IVF. For these reasons, some fertility specialists recommend that couples who fail to conceive after 2 to 3 cycles proceed directly to IVF.
In Vitro Fertilization (IVF)
Most ART procedures use IVF. An in vitro procedure is one that is performed in the laboratory. Advances in these procedures have dramatically increased the rate of live births. IVF can be performed with a woman's own eggs and sperm, or with donor eggs and sperm.
A standard IVF cycle is divided into the following steps:
Ovarian Suppression.
The woman receives treatment with either a GnRH agonist (Lupron) or GnRH antagonist (Antagon, Cetrotide). Sometimes birth control pills are given as pretreatment. The purpose is to prevent premature ovulation and make sure that the follicles will ripen at the same time.Ovarian Stimulation.
Ovarian-stimulating drugs, such as clomiphene, FSH, or LH, are used to prompt the ovaries to produce multiple eggs. The woman receives ultrasounds to monitor the growth of egg follicles and blood tests to check hormone levels. A cycle may be canceled if not enough follicles are produced or if there is a risk of OHSS (seeMedications
section).Trigger Injection of hCG.
About 8 to 14 days later, an injection of hCG is given to foster egg maturation. The timing of this shot is very important for the success of the IVF procedure.Egg Retrieval.
About 34 to 36 hours after the hCG injection, the eggs are retrieved. To retrieve the eggs, the doctor inserts an ultrasound-guided probe into the vagina. A needle is then used to drain the liquid from the follicles, and several eggs are retrieved. The woman begins taking progesterone or another type of medication to help prepare the lining of the uterus to support the embryo.Fertilization and Embryo Culture.
The doctor will examine the eggs to evaluate their quality and maturity. Selected eggs are placed in a culture in the laboratory and transferred to an incubator. They are then inseminated with sperm, either by placing sperm together with the egg or injecting a single sperm into the egg (intracytoplasmic sperm injection or ICSI procedure).Embryo Transfer and Cryopreservation.
One or more embryos are implanted in the woman's uterus 2 to 6 days after egg retrieval. The doctor will discuss with the woman the appropriate number of embryos to be implanted. Excess embryos may be frozen and saved for future use. It takes about 9 to 12 days to determine if pregnancy has been achieved.
Embryo Transfer Guidelines
The American Society for Reproductive Medicine (ASRM) and the Society for Assisted Reproductive Technologies (SART) have joint guidelines on the number of embryos that should be transferred during IVF procedures. The 2017 guidelines distinguish between cleavage-stage embryos (2 to 3 days after fertilization) and blastocyst embryos (5 to 6 days after fertilization). Apart from young age, the guidelines define the following characteristics as favorable prognosis: 1) expectation of one or more high-quality embryos available for cryopreservation; 2) euploid embryos; and 3) previous live birth after an IVF cycle. In people who do not meet criteria for a favorable prognosis in each of the below age groups, an additional embryo transfer may be considered.
For women with favorable prognosis, the 2017 guidelines recommend:
- For women under the age of 35 years, a single embryo transfer or no more than 2 embryos (either cleavage-stage or blastocyst)
- For women between ages 35 and 37 years, strong consideration should be made for a single cleavage-stage embryo transfer
- For women between ages 38 and 40 years, no more than 3 cleavage-stage embryos or 2 blastocysts
- For women ages 41 to 42 years, no more than 4 cleavage-stage embryos or 3 blastocysts
- For women older than age 43 years, there are insufficient data to recommend a limit on the number of embryos
These embryo numbers are recommended for women with favorable prognoses. For women who have failed to become pregnant after at least 2 IVF cycles, or who have a less favorable prognosis, the doctor may consider adding 1 additional embryo. The guidelines apply to both fresh and frozen embryos.
Success Rates
Not all IVF cycles result in pregnancy, and not all IVF-achieved pregnancies result in live births. When a woman's own eggs are used, results are better with fresh embryos than frozen embryos. Success rates depend on many factors, especially the age of the woman.
Data from SART in 2015 indicate that the chances of ART resulting in live birth are about:
- 54% for women younger than age 35 years
- 34% for women ages 35 to 37 years
- 23% for women ages 38 to 40 years
- 12% for women ages 41 to 42 years
- 4% for women older than age 42 years
Complications
Data have been conflicting on whether IVF increases the risk for genetic abnormalities and birth defects. In general, the overall risks for birth defects appear to be small. Studies indicate that most children conceived through IVF are healthy and have normal cognitive development and school performance. However, recent studies suggest that fetuses conceived with ICSI and IVF may have a higher risk of congenital heart defects.
The main risk of IVF is the consequences of multiple pregnancies. Multiple pregnancies increase the chance of health problems for a mother and her babies. In particular, there is increased risk for premature delivery and low birth weight. These factors can cause heart and lung problems and developmental disabilities in children.
Gamete Intrafallopian Transfer (GIFT) and Zygote Intrafallopian Transfer (ZIFT)
GIFT is a laparoscopic procedure by which both washed sperm from the male partner and eggs from the female partner are transferred to the fallopian tubes at the same time. Egg retrieval precedes GIFT in the same surgical event. GIFT is not an IVF procedure, since fertilization occurs in the fallopian tubes.
ZIFT is the laparoscopic transfer of zygotes (single cell stage of the embryo) to the fallopian tubes, 24 hours after IVF. ZIFT following all but the last step of IVF as described above.
GIFT and ZIFT are rarely performed due to the requirement for laparoscopy. Studies have not proven them to be more successful compared to traditional IVF.
Intracytoplasmic Sperm Injection (ICSI)
ICSI is an ART used for couples when male infertility is the main problem. It involves injecting a single sperm into an egg obtained from IVF.
The procedure is very simple:
- A tiny glass tube (called a holding pipet) stabilizes the egg.
- A second glass tube (called the injection pipet) is used to penetrate the egg's membrane and deposit a single sperm into the egg.
- The egg is released into a drop of cultured medium.
- If fertilized, the egg is allowed to develop for 1 to 2 days, then it is either frozen or implanted.
The greatest concern with this procedure has been whether it increases the risk for birth defects. Many, but not all, studies have reported no higher risks of birth defects in children born using ICSI procedures. However, if the father's infertility was due to genetic issues, this genetic defect may be passed on to male children conceived through ICSI.
Another concern has been whether the ICSI procedure is being overused. Some doctors recommend ICSI for women who have failed prior IVF attempts or who have few or poor-quality eggs, even if their male partners have normal semen measurements. According to the SART, there is little evidence that ICSI helps improve pregnancy success for couples who do not have a problem with male factor infertility.
Lifestyle Changes
Although there are no dietary or nutritional cures for infertility, a healthy lifestyle is important. Some ovulatory problems may be helped by changing behavioral patterns. Some tips include:
- Maintain a healthy weight. Women who are either overweight or underweight are at risk for fertility failure, including a lower chance for achieving success with fertility procedures. Choosing a healthy diet is an important part of the process.
- Stop smoking. Smoking adversely affects infertility in both men and women and may affect the success of fertility treatments. Everyone should quit.
- Avoid excessive exercise if it causes menstrual irregularity. However, moderate and regular exercise is essential for good health.
- Limit excessive caffeine and alcohol consumption. High levels of alcohol and caffeine are associated with decreased fertility.
- Avoid most commercial water-based sexual lubricants (Astroglide, KY Jelly). They can interfere with sperm motility and survival.
- Avoid any unnecessary medications.
Planning Sexual Activity
The Fertile Window
An egg survives only 12 to 24 hours after it is released from the ovary. For conception to occur, a sperm must be able to fertilize the egg during this time. Couples can optimize their chances for conception by planning sexual intercourse during the woman's fertile window:
- The fertile window is 6 days long, starts 5 days before ovulation, and ends the day of ovulation.
- In a woman with a 28-day menstrual cycle, ovulation usually occurs around day 14 (14 days after the start of her menstrual period), which means the fertile window occurs from days 9 to 14. However, the length of menstrual cycles, and fertile windows, vary from woman to woman.
- The chances for intercourse resulting in pregnancy are considered to be highest during the fertile window and especially on the 3-day interval that ends on the day of ovulation.
Diagnosis
section of this report).Frequency of Intercourse
Evidence indicates that chances are best for conception when sexual intercourse occurs every 1 to 2 days, especially during the fertile window. Less frequent sexual intercourse (2 to 3 times a week) also achieves good results. However, couples need to make their own personal choices about what amount of sexual activity is appropriate, comfortable, and desirable. Data suggests that abstinence (not having sex) of more than 5 to 10 days may adversely affect sperm health.
Sexual Practices
There is no evidence that any particular sexual positions, or resting after sex, help increase the chances for pregnancy. There is also no evidence that whether or not a woman achieves orgasm affects the likelihood of her becoming pregnant. Couples should be aware that water-based vaginal lubricants (Astroglide, K-Y Jelly, saliva) can damage sperm's ability to swim and should not be used. For lubrication, try mineral oil, canola oil, or commercially available "fertility friendly" products such as Pre-Seed, which do not harm sperm.
Dealing with Stress
The fertility treatment process presents a roller coaster of emotions. There are almost no sure ways to predict which couples will eventually conceive. Some couples with multiple problems will overcome great odds, while other, seemingly fertile, couples fail to conceive. Many of the new treatments are remarkable, but a live birth is never guaranteed. The emotional burden on the couple is considerable, and some planning is helpful. You should:
- Decide in advance how many and what kind of procedures will be emotionally and financially acceptable and attempt to determine a final limit. Fertility treatments can be expensive. A successful pregnancy often depends on repeated attempts.
- Prepare for multiple births as a possible outcome for successful pregnancy. A pregnancy that results in a multiple birth introduces new complexities and emotional problems.
- Determine alternatives (adoption, donor sperm or egg, or having no children) as early as possible in the fertility process. This can reduce anxiety during treatments and feelings of disappointment in case conception does not occur.
On a reassuring note, studies on infertility in women indicate that stress levels do not affect the outcome of fertility treatments. There appears to be no difference in stress levels between women who become pregnant and those who do not. Women who are feeling stressed by problems with fertility or the challenges of the fertility treatment process should not feel additionally concerned that their emotional state may affect their chances of becoming pregnant.
Resources
- American Society for Reproductive Medicine -- www.asrm.org
- Society for Assisted Reproductive Technology -- www.sart.org
- Path2Parenthood -- www.path2parenthood.org
- American College of Obstetricians and Gynecologists -- www.acog.org
- Centers for Disease Control and Prevention: Reproductive Health -- www.cdc.gov/reproductivehealth/index.htm
References
Barbieri RL. Female infertility. In: Strauss JF, Barbieri RL, eds. Yen & Jaffe's Reproductive Endocrinology. 8th ed. Elsevier; 2019:chap 22.
Broekmans FJ, Fauser BCJM. Female infertility: evaluation and management. In: Jameson JL, De Groot LJ, de Kretser DM, et al, eds. Endocrinology: Adult and Pediatric. 7th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 132.
Catherino WH. Reproductive endocrinology and infertility. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier Saunders; 2020:chap 223.
Centers for Disease Control and Prevention website. ART success rates. www.cdc.gov/art/artdata/index.html. Updated November 15, 2019. Accessed February 25, 2020.
Choi J, Lobo RA. In vitro fertilization. In: Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 43.
Donnez J, Dolmans MM. Fertility preservation in women. N Engl J Med. 2017;377(17):1657-1665. PMID: 29069558 pubmed.ncbi.nlm.nih.gov/29069558.
Gavin L, Pazol K, Ahrens K. Update: providing quality family planning services - recommendations from CDC and the US Office of Population Affairs, 2017. MMWR Morb Mortal Wkly Rep. 2017;66(50):1383-1385. PMID: 29267259 pubmed.ncbi.nlm.nih.gov/29267259.
Giorgione V, Parazzini F, Fesslova V, et al. Congenital heart defects in IVF/ICSI pregnancy: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(1):33-42. PMID: 29164811 pubmed.ncbi.nlm.nih.gov/29164811.
Hornstein MD. State of the ART: assisted reproductive technologies in the United States. Reprod Sci. 2016;23(12):1630-1633. PMID: 27624310 pubmed.ncbi.nlm.nih.gov/27624310.
Kamath MS, Maheshwari A, Bhattacharya S, Lor KY, Gibreel A. Oral medications including clomiphene citrate or aromatase inhibitors with gonadotropins for controlled ovarian stimulation in women undergoing in vitro fertilisation. Cochrane Database Syst Rev. 2017;11:CD008528. PMID: 29096046 pubmed.ncbi.nlm.nih.gov/29096046.
Lindsay TJ, Vitrikas KR. Evaluation and treatment of infertility. Am Fam Physician. 2015;91(5):308-314. PMID: 25822387 pubmed.ncbi.nlm.nih.gov/25822387.
Lobo RA. Infertility: etiology, diagnostic evaluation, management, prognosis. In: Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 42.
Luke B. Pregnancy and birth outcomes in couples with infertility with and without assisted reproductive technology: with an emphasis on US population-based studies. Am J Obstet Gynecol. 2017;217(3):270-281. PMID: 28322775 pubmed.ncbi.nlm.nih.gov/28322775.
Nelson SM. Prevention and management of ovarian hyperstimulation syndrome. Thromb Res. 2017;151 Suppl 1:S61-S64. PMID: 28262238 pubmed.ncbi.nlm.nih.gov/28262238.
Oktay K, Harvey BE, Partridge AH, et al. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2018;36(19):1994-2001. PMID: 29620997 pubmed.ncbi.nlm.nih.gov/29620997.
Practice Committee of the American Society for Reproductive Medicine. Diagnostic evaluation of the infertile female: a committee opinion. Fertil Steril. 2015;103(6):e44-e50. PMID: 25936238 pubmed.ncbi.nlm.nih.gov/25936238.
Practice Committee of the American Society for Reproductive Medicine; Practice Committee of the Society for Assisted Reproductive Technology. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2017;107(4):901-903. PMID: 28292618 pubmed.ncbi.nlm.nih.gov/28292618.
Practice Committee of the American Society for Reproductive Medicine. Prevention and treatment of moderate and severe ovarian hyperstimulation syndrome: a guideline. Fertil Steril. 2016;106(7):1634-1647. PMID: 27678032 pubmed.ncbi.nlm.nih.gov/27678032.
Practice Committee of the American Society for Reproductive Medicine. Role of metformin for ovulation induction in infertile patients with polycystic ovary syndrome (PCOS): a guideline. Fertil Steril. 2017;108(3):426-441. PMID: 28865539 pubmed.ncbi.nlm.nih.gov/28865539.
Tsen LC. In vitro fertilization and other assisted reproductive technology. In: Chestnut DH, Wong CA, Tsen LC, et al, eds. Chestnut's Obstetric Anesthesia: Principles and Practice. 6th ed. Elsevier; 2020:chap 15.
Review Date: 3/23/2020
Reviewed By: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.