Health Library
Colorectal cancer
Colorectal cancer; Cancer - colon; Rectal cancer; Cancer - rectum; Adenocarcinoma - colon; Colon - adenocarcinoma; Colon carcinoma; Colon cancer
Colorectal cancer is cancer that starts in the large intestine (colon) or the rectum (end of the colon). It is also sometimes simply called colon cancer.
In the United States, colorectal cancer is one of the leading causes of deaths due to cancer. Early diagnosis can often lead to a complete cure.
Images








Presentation



I Would Like to Learn About:
Causes
Nearly all colorectal cancers begin as noncancerous (benign) lumps (polyps) in the lining of the colon and rectum. These can slowly develop into cancer.
You have a higher risk for colorectal cancer if you:
- Are age 45 or older
- Drink alcohol
- Smoke tobacco
- Are overweight or have obesity
- Are African American or of eastern European descent
- Eat a lot of red or processed meats
- Eat a low-fiber and high-fat diet
- Have a diet low in fruits and vegetables
- Have colorectal polyps
- Have inflammatory bowel disease (Crohn disease or ulcerative colitis)
- Have a family history of colorectal cancer
Some inherited diseases also increase the risk of developing colorectal cancer. One of the most common is called Lynch syndrome.
Symptoms
Many cases of colon cancer have no symptoms. If there are symptoms, the following may indicate colon cancer:
- Abdominal pain and tenderness in the lower abdomen
- Blood in the stool
- Diarrhea, constipation, or other change in bowel habits
- Narrow stools
- Weight loss with no known reason
Exams and Tests
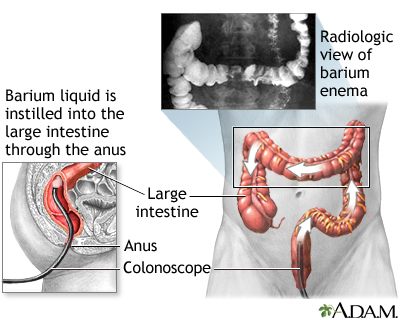
Through screening tests, colon cancer can be detected before symptoms develop. This is when the cancer is most curable. Abnormal stool screening tests should be followed up with a colonoscopy, which can see the entire colon.
Your health care provider will perform a physical exam and press on your belly area. The physical exam rarely shows any problems, although your provider may feel a lump (mass) in the abdomen. A rectal exam may reveal a mass in people with rectal cancer, but not colon cancer.
Blood tests may be done for those diagnosed with colorectal cancer, including:
- Complete blood count (CBC) to check for anemia
- Liver function tests
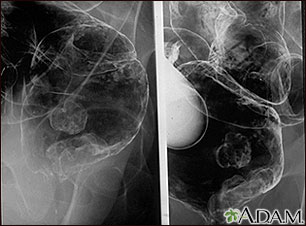
If you are diagnosed with colorectal cancer, more tests will be done to see if the cancer has spread. This is called staging. CT or MRI scans of the abdomen, pelvic area, or chest may be used to stage the cancer. Sometimes, PET scans are also used.
Stages of colorectal cancer are:
- Stage 0: Cancer is only on the innermost layer of the lining of the intestine
- Stage I: Cancer is in the inner layers of the colon
- Stage II: Cancer has spread through the muscle wall of the colon
- Stage III: Cancer has spread to the lymph nodes
- Stage IV: Cancer spread to other organs, such as the liver or lungs
Blood tests to detect tumor markers, such as carcinoembryonic antigen (CEA) may help your provider monitor your progress during and after treatment.
Treatment
Treatment depends on many things, including the stage of the cancer. Treatments may include:
- Endoscopic surgery (less invasive surgery using a lighted, flexible tube)
- Surgery
- Chemotherapy
- Radiation therapy
- Immunotherapy
- Targeted therapy
SURGERY
Stage 0 colon cancer may be treated by removing the tumor using endoscopic surgery (colonoscopy). For stages I, II, and III cancer, more extensive surgery is needed to remove all or part of the colon and rectum that is cancerous. This surgery is called colon resection (colectomy).
CHEMOTHERAPY
Chemotherapy involves taking medicines that kill cancer cells. You may receive just one type of medicine or a combination of medicines.
Most people with stage III colon cancer receive chemotherapy after surgery for 3 to 6 months. This is called adjuvant chemotherapy. Even though the tumor was removed, chemotherapy is given to treat any cancer cells that may remain.
Chemotherapy is also used to improve symptoms and prolong survival in people with stage IV colon cancer.
IMMUNOTHERAPY
Immunotherapy involves taking medicines that increase the ability of your own immune system to destroy cancer cells. Immunotherapy has different side effects than chemotherapy.
RADIATION
Radiation therapy involves using radiation to kill cancer cells. Radiation therapy is often used in the treatment of rectal cancer.
TARGETED THERAPY
- Targeted treatment zeroes in on specific targets (molecules) in cancer cells. These targets play a role in how cancer cells grow and survive. Using these targets, the drug disables the cancer cells so they cannot spread. Targeted therapy may be given as pills or may be injected into a vein.
- You may have targeted therapy along with surgery, chemotherapy, or radiation treatment.
CANCER IN THE LIVER
For people with stage IV disease that has spread to the liver, treatment can be directed at the cancer tumors in the liver. This may include:
- Burning the liver tumors (ablation)
- Delivering chemotherapy or radiation directly into the liver
- Freezing the liver tumors (cryotherapy)
- Surgery
- Radioactive beads/spheres that deliver treatment to kill the cancer cells
- Alcohol (ethanol) injected into the liver tumors to kill cancer cells
Support Groups
You can ease the stress of the disease by joining a colon cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
With treatment, stages 0, I, II, and III cancers often are cured, although higher stages of cancer are less likely to be cured. In most cases, stage IV cancer is not curable, but there are exceptions, including sometimes when the spread of the cancer is limited to the liver. In order for a person to be cured, treatment must get rid of all of the cancer. But there is a chance that the cancer will come back. If this occurs, curing the cancer is much less likely than before.
Cancer treatment can cause problems such as:
- Bowel obstruction from surgical scarring.
- Many sorts of short- and long-term side effects from chemotherapy, immunotherapy, radiation, and therapy targeted to the liver.
Possible Complications
Complications may include:
- Blockage of the colon, causing bowel obstruction
- Cancer returning in the colon
- Cancer spreading to other organs or tissues (metastasis)
- Development of a second primary colorectal cancer
When to Contact a Medical Professional
Contact your provider if you have:
- Black, tar-like stools
- Blood during a bowel movement
- Change in bowel habits
- Unexplained weight loss
Prevention
Colon cancer can almost always be caught by colonoscopy in early stages, when it is most curable. All adults age 45 and older should have a colon cancer screening. How often you should have screening depends upon the test being used.
Colon cancer screening can often find polyps before they become cancerous. Removing these polyps may prevent colon cancer.
People with certain risk factors for colon cancer may need earlier testing (before age 45) or more frequent testing.
A healthy lifestyle also may help reduce your risk for colon cancer:
- Get regular physical activity.
- Don't smoke or use tobacco.
- Maintain a healthy weight.
- Eat a diet rich in fruits and vegetables and low in red and processed meats.
Related Information
CancerHodgkin lymphoma
Melanoma
Colorectal polyps
Ulcerative colitis
Metastasis
Virtual colonoscopy
Ileostomy
Total proctocolectomy and ileal-anal pouch
Total proctocolectomy with ileostomy
Chemotherapy - what to ask your doctor
Radiation therapy - questions to ask your doctor
Changing your ostomy pouch
Ileostomy - what to ask your doctor
Abdominal radiation - discharge
Pelvic radiation - discharge
Bland diet
Ileostomy and your child
Ileostomy and your diet
Ileostomy - caring for your stoma
Ileostomy - changing your pouch
Types of ileostomy
Ileostomy - discharge
Living with your ileostomy
Large bowel resection - discharge
Small bowel resection - discharge
Total colectomy or proctocolectomy - discharge
References
Centers for Disease Control and Prevention website. Reducing risk for colorectal cancer. www.cdc.gov/colorectal-cancer/prevention/. Updated June 20, 2024. Accessed August 27, 2024.
Garber JJ, Chung DC. Colonic polyps and polyposis syndromes. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 126.
Lawler M, Johnston B, Van Schaeybroeck S, et al. Colorectal cancer. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 74.
National Cancer Institute website. Colorectal Cancer Prevention (PDQ) - Health Professional Version. www.cancer.gov/types/colorectal/hp/colorectal-prevention-pdq. Updated March 28, 2024. Accessed August 27, 2024.
National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology (NCCN guidelines): colorectal cancer screening. Version 1.2024 - February 27, 2024. www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf. Updated February 27, 2024. Accessed August 27, 2024.
Patel SG, May FP, Anderson JC, et al. Updates on age to start and stop colorectal cancer screening: recommendations from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2022;117(1):57-69. PMID: 34962727 pubmed.ncbi.nlm.nih.gov/34962727/.
Qaseem A, Crandall CJ, Mustafa RA, et al. Screening for colorectal cancer in asymptomatic average-risk adults: a guidance statement from the American College of Physicians. Ann Intern Med. 2019;171(9):643-654. PMID: 31683290 pubmed.ncbi.nlm.nih.gov/31683290/.
US Preventive Services Task Force website. Final recommendation statement. Colorectal cancer: screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening. Published May 18, 2021. Accessed February 11, 2024.
BACK TO TOPReview Date: 4/18/2023
Reviewed By: John Roberts, MD, Professor of Internal Medicine (Medical Oncology), Yale Cancer Center, New Haven, CT. He is board certified in Internal Medicine, Medical Oncology, Pediatrics, Hospice and Palliative Medicine. Review provided by VeriMed Healthcare Network. Internal review and update on 02/20/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 08/27/2024.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
