Blastomycosis
North American blastomycosis; Gilchrist disease
Blastomycosis is an infection caused by breathing in the Blastomyces dermatitidis fungus. The fungus is found in decaying wood and soil.
Causes
You can get blastomycosis by contact with moist soil, most commonly where there is rotting wood and leaves. The fungus enters the body through the lungs, where the infection starts. The fungus can then spread to other parts of the body. The disease may affect the skin, bones and joints, and other areas.
Blastomycosis is rare. It is found in the central and southeastern United States, and in Canada, India, Israel, Saudi Arabia, and Africa.
The key risk factor for the disease is contact with infected soil. It most often affects people with weakened immune systems, such as those with HIV/AIDS or who have had an organ transplant, but it can also infect healthy people. Men are more likely to be affected than women.
Symptoms
Lung infection may not cause any symptoms. Symptoms may be seen if the infection spreads. Symptoms may include:
- Joint pain
- Chest pain
- Cough (may produce brown or bloody mucus)
- Fatigue
- Fever
- Night sweats
- General discomfort, uneasiness, or ill feeling (malaise)
- Muscle pain
- Unintentional weight loss
Most people develop skin symptoms when the infection spreads. You may get papules, pustules, or nodules on exposed body areas.
The pustules:
- May look like warts or ulcers
- Are usually painless
- Vary in color from gray to violet
- May appear in the nose and mouth
- Bleed easily and form ulcers
Exams and Tests
The health care provider will perform a physical examination. You'll be asked about your medical history and symptoms.
If the provider suspects you have a fungal infection, diagnosis can be confirmed by these tests:
- Chest CT scan
- Chest x-ray
- Skin biopsy
- Sputum culture and examination
- Urinary antigen detection
- Tissue biopsy and culture
- Urine culture
Treatment
You may not need to take medicine for a mild blastomycosis infection that stays in the lungs. The provider may recommend the following antifungal medicines when the disease is severe or spreads outside of the lungs.
- Fluconazole
- Itraconazole
- Ketoconazole
Amphotericin B may be used for severe infections.
Follow up regularly with your provider to make sure the infection does not return.
Outlook (Prognosis)
People with minor skin sores (lesions) and mild lung infections usually recover completely. The infection can lead to death if not treated.
Possible Complications
Complications of blastomycosis may include:
- Large sores with pus (abscesses)
- Skin sores can lead to scarring and loss of skin color (pigment)
- Return of the infection (relapse or disease recurrence)
- Side effects from drugs such as amphotericin B
When to Contact a Medical Professional
Contact your provider if you have symptoms of blastomycosis.
Prevention
Avoiding travel to areas where the infection is known to occur may help prevent exposure to the fungus, but this may not always be possible.
References
Elewski BE, Hughey LC, Hunt KM, Hay RJ. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 77.
Gauthier GM, Klein BS. Blastomycosis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 264.
Kauffman CA, Galagiani JN, Thompson GR. Endemic mycoses. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 316.
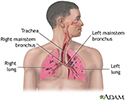
Respiratory system - illustration
Respiratory system
illustration
Fungus - illustration
Fungus
illustration
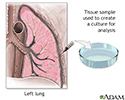
Lung tissue biopsy - illustration
Lung tissue biopsy
illustration
Osteomyelitis - illustration
Osteomyelitis
illustration
Review Date: 9/10/2022
Reviewed By: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.