Simple pulmonary eosinophilia
Pulmonary infiltrates with eosinophilia; Loffler syndrome; Eosinophilic pneumonia; Pneumonia - eosinophilic
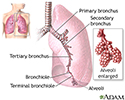
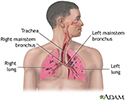
Simple pulmonary eosinophilia is inflammation of the lungs from an increase in eosinophils, a type of white blood cell. Pulmonary means related to the lungs.
Causes
Most cases of this condition are due to an allergic reaction from:
- A medicine, such as a sulfonamide antibiotic or a non-steroidal anti-inflammatory drug (NSAID), such as ibuprofen or naproxen
- Infection with a fungus such as Aspergillus fumigatus or Pneumocystis jirovecii
- A parasite, including the roundworms Ascariasis lumbricoides, or Necator americanus , or the hookworm Ancylostoma duodenale
In some cases, no cause is found.
Symptoms
Symptoms may include any of the following:
Symptoms can range from none at all to severe. They may go away without treatment.
Exams and Tests
The health care provider will listen to your chest with a stethoscope. Crackle-like sounds, called rales, may be heard. Rales suggest inflammation of the lung tissue.
A complete blood count (CBC) test may show increased white blood cells, particularly eosinophils.
Chest x-ray usually shows abnormal shadows called infiltrates. They may disappear with time or reappear in different areas of the lung.
A bronchoscopy with washing usually shows a large number of eosinophils.
A procedure that removes the stomach contents (gastric lavage) may show signs of the ascaris worm or another parasite.
Treatment
If you are allergic to a medicine, your provider may tell you to stop taking it. Never stop taking a medicine without first talking with your provider.
If the condition is due to an infection, you may be treated with an antibiotic or antiparasitic medicine.
Sometimes, anti-inflammatory medicines called corticosteroids are given, especially if you have aspergillosis.
Outlook (Prognosis)
The disease often goes away without treatment. If treatment is needed, the response is usually good. But, the disease can come back, especially if the condition does not have a specific cause and needs to be treated with corticosteroids.
Possible Complications
A rare complication of simple pulmonary eosinophilia is a severe type of pneumonia called acute idiopathic eosinophilic pneumonia.
When to Contact a Medical Professional
See your provider if you have symptoms that may be linked with this disorder.
Prevention
This is a rare disorder. Many times, the cause cannot be found. Minimizing exposure to possible risk factors, such as certain medicines or parasites, may reduce the chance of developing this disorder.
References
Cottin V. Eosinophilic lung diseases. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 96.
Khoury P, Akuthota P, Weller PF, Klion AD. Eosinophilia and eosinophil-related disorders. In: Burks AW, Holgate ST, O'Hehir RE, et al, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 73.
Kim K, Weiss LM. Parasitic infections. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 58.
Review Date: 5/3/2023
Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron Jr. Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.