Bile duct obstruction
Biliary obstruction
Bile duct obstruction is a blockage in the tubes that carry bile from the liver to the gallbladder and small intestine.
Causes
Bile is a liquid released by the liver. It contains cholesterol, bile salts, and waste products such as bilirubin. Bile salts help your body break down (digest) fats. Bile passes out of the liver through the bile ducts and is stored in the gallbladder. After a meal, it is released into the small intestine.
When the bile ducts become blocked, bile builds up in the liver, and jaundice (yellow color of the skin) develops due to the increasing level of bilirubin in the blood.
The possible causes of a blocked bile duct include:
- Cysts of the common bile duct
- Enlarged lymph nodes in the porta hepatis
- Gallstones
- Inflammation of the bile ducts
- Narrowing of the bile ducts from scarring
- Injury from gallbladder surgery
- Tumors of the bile ducts or pancreas
- Tumors that have spread to the biliary system
- Liver and bile duct worms (flukes)
The risk factors for a blocked bile duct include:
- History of gallstones, chronic pancreatitis, or pancreatic cancer
- Injury to the abdominal area
- Recent biliary surgery
- Recent biliary cancer (such as bile duct cancer)
The blockage can also be caused by infections. This is more common in people with weakened immune systems.
Symptoms
Symptoms may include:
- Abdominal pain in the upper right side
- Dark urine
- Fever
- Itching
- Jaundice (yellow skin color)
- Nausea and vomiting
- Clay-colored or pale stools
Exams and Tests
Your health care provider will examine you and feel your belly.
The following blood test results could be due to a possible blockage:
- Increased bilirubin level
- Increased alkaline phosphatase level
- Increased GGT enzyme level
- Increased liver enzymes
The following tests may be used to investigate a possible blocked bile duct:
- Abdominal ultrasound
- Abdominal CT scan
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Percutaneous transhepatic cholangiogram (PTCA)
- Magnetic resonance cholangiopancreatography (MRCP)
- Endoscopic ultrasound (EUS)
A blocked bile duct may also alter the results of the following tests:
- Amylase blood test
- Gallbladder radionuclide scan
- Lipase blood test
- Prothrombin time (PT)
- Urine bilirubin
Treatment
The goal of treatment is to relieve the blockage. Stones may be removed using an endoscope during an ERCP.
In some cases, surgery is required to bypass the blockage. The gallbladder will usually be surgically removed if the blockage is caused by gallstones. Your provider may prescribe antibiotics if an infection is suspected.
If the blockage is caused by cancer, the duct may need to be widened. This procedure is called endoscopic or percutaneous (through the skin next to the liver) dilation. A tube may need to be placed to allow drainage.
Outlook (Prognosis)
If the blockage is not corrected, it can lead to life-threatening infection and a dangerous buildup of bilirubin.
If the blockage lasts a long time, chronic liver disease can result. Most obstructions can be treated with endoscopy or surgery. Obstructions caused by cancer often have a worse outcome.
Possible Complications
Left untreated, the possible complications include infections, sepsis, and liver disease, such as biliary cirrhosis.
When to Contact a Medical Professional
Contact your provider if you:
- Notice a change in the color of your urine and stools
- Develop jaundice
- Have abdominal pain that doesn't go away or keeps recurring
Prevention
Be aware of any risk factors you have, so that you can get prompt diagnosis and treatment if a bile duct becomes blocked. The blockage itself may not be preventable.
References
Fogel EL, Sherman S. Diseases of the gallbladder and bile ducts. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 146.
Lidofsky SD. Jaundice. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 21.
Digestive system - illustration
Digestive system
illustration
Endocrine glands - illustration
Endocrine glands
illustration
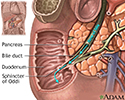
Bile pathway - illustration
Bile pathway
illustration
Biliary obstruction - series - Normal anatomy
Presentation
Review Date: 5/4/2022
Reviewed By: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.