Waldenstrom macroglobulinemia
Waldenström macroglobulinemia; Macroglobulinemia - primary; Lymphoplasmacytic lymphoma; Monoclonal macroglobulinemia; Waldenström macroglobulinemia
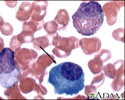
Waldenström macroglobulinemia (WM) is a cancer of the B lymphocytes (a type of white blood cell). WM is associated with the overproduction of proteins called IgM antibodies.
Causes
WM is a result of a condition called lymphoplasmacytic lymphoma. This is a cancer of the white blood cells, in which the B immune cells start dividing rapidly. The exact cause of too much production of the IgM antibody is unknown. Hepatitis C may increase the risk of WM. Gene mutations are often found in the malignant B cells.
Production of excess IgM antibodies can cause several types of problems:
- Hyperviscosity, which causes the blood to become too thick. This can make it harder for blood to flow through small blood vessels.
- Neuropathy, or nerve damage, when the IgM antibody damages nerve tissue.
- Anemia, when the IgM antibody binds to red blood cells and damages them.
- Kidney disease, when the IgM antibody deposits in kidney tissue.
- Cryoglobulinemia and vasculitis (inflammation of the blood vessels) when the IgM antibody forms immune complexes with cold exposure.
WM is very rare. Most people with this condition are over 65 years of age.
Symptoms
Symptoms of WM may include any of the following:
- Bleeding of the gums and nosebleeds
- Blurred or decreased vision
- Bluish skin in the fingers after cold exposure
- Dizziness or confusion
- Easy bruising of the skin
- Fatigue
- Diarrhea
- Numbness, tingling, or burning pain in the hands, feet, fingers, toes, ears, or nose
- Rash
- Swollen glands
- Unintentional weight loss
- Vision loss in one eye
Exams and Tests
A physical exam may reveal a swollen spleen, liver, and lymph nodes. An eye exam may show enlarged veins in the retina or retinal bleeding (hemorrhages).
A complete blood count (CBC) may show a low number of red blood cells or platelets. Blood chemistry may show evidence of kidney disease.
A blood test called serum protein electrophoresis shows an increased level of the IgM antibody. Levels are often higher than 3000 milligrams per deciliter (mg/dL), or 30 grams per liter (g/L). An immunofixation test will be done to show if the IgM antibody is derived from a single cell type (clonal).
A serum viscosity test can tell if the blood has become thick. Symptoms usually occur when the blood is four times thicker than normal.
A bone marrow biopsy will show increased numbers of abnormal cells that look like both lymphocytes and plasma cells.
Additional tests that may be done include:
- 24-hour urine protein
- Total protein
- Immunofixation in urine
- T (thymus derived) lymphocyte count
- Bone x-rays
Treatment
Some people with WM who have increased IgM antibodies do not have symptoms. This condition is known as smoldering WM. No treatment is needed other than careful follow-up.
In people with symptoms, treatment aims at decreasing the symptoms and the risk of developing organ damage. There is no current standard treatment. Your health care provider may suggest that you participate in a clinical trial.
Plasmapheresis removes IgM antibodies from the blood. It also controls the symptoms caused by blood thickening.
Medicines may include corticosteroids, a combination of chemotherapy medicines and the monoclonal antibody to B cells, rituximab.
Autologous stem cell transplant may be recommended for some people with otherwise good health.
People who have a low number of red or white blood cells or platelets may need transfusions or antibiotics.
Outlook (Prognosis)
The average survival is about 5 years. Some people live more than 10 years.
In some people, the disorder may produce few symptoms and progress slowly.
Possible Complications
Complications of WM may include:
- Changes in mental function, possibly leading to coma
- Heart failure
- Gastrointestinal bleeding or malabsorption
- Vision problems
- Hives
When to Contact a Medical Professional
Contact your provider if symptoms of WM develop.
References
Castillo JJ, Treon SP. Waldenström macroglobulinemia/lymphoplasmacytic lymphoma. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 92.
Kapoor P, Ansell SM, Fonseca R, et al. Diagnosis and management of Waldenström macroglobulinemia: Mayo stratification of macroglobulinemia and risk-adapted therapy (mSMART) guidelines 2016. JAMA Oncol. 2017;3(9):1257-1265. PMID: 28056114 pubmed.ncbi.nlm.nih.gov/28056114/.
Rajkumar SV. Plasma cell disorders. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 173.
Review Date: 5/9/2024
Reviewed By: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, NY and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.