Cerebral palsy
Spastic paralysis; Paralysis - spastic; Spastic hemiplegia; Spastic diplegia; Spastic quadriplegia
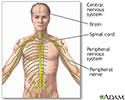
Cerebral palsy (CP) is a group of disorders that involve the brain. This affects nervous system functions, such as movement, learning, hearing, seeing, and thinking.
There are several different types of CP, including spastic, dyskinetic, ataxic, hypotonic, and mixed.
Causes
CP is caused by injuries or abnormalities of the brain. Most of these problems occur as the baby grows in the womb. But they can happen at any time during the first 2 years of life, while the baby's brain is still developing.
In some people with cerebral palsy, parts of the brain are injured due to a low level of oxygen (hypoxia) in those areas. It is not known why this occurs.
Premature infants have a slightly higher risk of developing CP. It may also occur in early infancy as a result of certain conditions such as:
- Bleeding in the brain
- Brain infections (encephalitis, meningitis, herpes simplex infections)
- Head injury
- Infections in the mother during pregnancy (rubella)
- Untreated jaundice
- Injuries to the brain during the childbirth process
- Exposure to toxins while developing (mercury)
In some cases, the cause of CP is never determined.
Symptoms
Symptoms of CP can be very different between people with this group of disorders. Symptoms may:
- Be very mild or very severe
- Only involve one side of the body or both sides
- Be more pronounced in either the arms or legs, or involve both the arms and legs
Symptoms are usually seen before a child is 2 years old. Sometimes symptoms begin as early as 3 months. Parents may notice that their child is delayed in reaching developmental stages such as sitting, rolling, crawling, or walking.
There are several different types of cerebral palsy. Some people have a mix of symptoms.
Spastic CP is the most common type. Symptoms include:
- Muscles that are very tight and do not stretch. They may tighten even more over time.
- Abnormal walk (gait) -- arms tucked in toward the sides, knees crossed or touching, legs make "scissors" movements, walk on the toes.
- Joints are tight and do not open all the way (called joint contracture).
- Muscle weakness or loss of movement in a group of muscles (paralysis).
- Symptoms may affect one arm or leg, one side of the body, both legs, or both arms and legs.
The following symptoms may occur in other types of CP:
- Abnormal movements (twisting, jerking, or writhing) of the hands, feet, arms, or legs while awake, which gets worse during periods of stress
- Tremors
- Unsteady gait
- Loss of coordination
- Floppy muscles, especially at rest, and joints that move around too much
Other brain and nervous system symptoms may include:
- Learning disabilities are common, but intelligence can be normal
- Speech problems (dysarthria)
- Hearing or vision problems
- Seizures
- Pain, especially in adults, which can be difficult to manage
Eating and digestion symptoms:
- Difficulty sucking or feeding in infants, or chewing and swallowing in older children and adults
- Vomiting or constipation
Other symptoms:
- Increased drooling
- Slower than normal growth
- Irregular breathing
- Urinary incontinence
Exams and Tests
Your health care provider will perform a full neurologic exam. In older people, testing cognitive function is also important.
Other tests may be performed as needed, most often to rule out other disorders:
- Blood tests
- CT scan of the head
- Cranial ultrasound (especially in pre-term infants)
- Electroencephalogram (EEG)
- Hearing screen
- MRI of the head
- Vision testing
Treatment
There is no cure for CP. The goal of treatment is to help the person be as independent as possible.
Treatment requires a team approach, including:
- Primary care provider
- Dentist (dental check-ups are recommended around every 6 months)
- Social worker
- Nurses
- Occupational, physical, and speech therapists
- Other specialists, including a neurologist, rehabilitation physician (physiatrist), pulmonologist, and gastroenterologist
Treatment is based on the person's symptoms and the need to prevent complications.
Self and home care include:
- Getting enough food and nutrition
- Keeping the home safe
- Performing exercises recommended by the providers
- Practicing proper bowel care (stool softeners, fluids, fiber, laxatives, regular bowel habits)
- Protecting the joints from injury
Putting the child in regular schools is recommended unless physical disabilities or mental development makes this impossible. Special education or schooling may help.
The following may help with communication and learning:
- Glasses
- Hearing aids
- Muscle and bone braces
- Walking aids
- Wheelchairs
Physical therapy, occupational therapy, orthopedic help, or other treatments may also be needed to help with daily activities and care.
Medicines may include:
- Anticonvulsants to prevent or reduce the frequency of seizures
- Botulinum toxin to help with spasticity and drooling
- Muscle relaxants to reduce tremors and spasticity
Surgery may be needed in some cases to:
- Control gastroesophageal reflux
- Cut certain nerves from the spinal cord to help with pain and spasticity
- Place a pump for medicine administration into spinal canal
- Place a feeding tube
- Release joint contractures
Shockwave therapy to reduce spasticity is being investigated.
Support Groups
Stress and burnout among parents and other caregivers of people with cerebral palsy is common. Seek support and more information from organizations that specialize in CP.
Outlook (Prognosis)
CP is a life-long disorder. Long-term care may be required. The disorder does not affect expected length of life. The amount of disability varies. Babies with mild CP may outgrow their symptoms.
Many adults are able to live in the community, either independently or with different levels of help.
Possible Complications
CP may lead to the following health problems:
- Bone thinning (osteoporosis)
- Bowel obstruction
- Hip dislocation and arthritis in the hip joint
- Injuries from falls
- Pressure sores
- Joint contractures
- Pneumonia caused by choking
- Poor nutrition
- Reduced communication skills (sometimes)
- Reduced intellect (sometimes)
- Scoliosis
- Seizures (in about half of the people who are affected by cerebral palsy)
- Social stigma
When to Contact a Medical Professional
Contact your provider if symptoms of CP develop, especially if you know that an injury occurred during birth or early infancy.
Prevention
Getting the proper prenatal care may reduce the risk for some rare causes of CP. In most cases though, the injury causing the disorder is not preventable.
Pregnant mothers with certain medical conditions may need to be followed in a high-risk prenatal clinic.
Adults with CP should continue to follow-up with a neurologist to reduce the risk of late complications.
References
Greenberg JM, Narendran V, Brady JM, Nathan AT, Haberman BB. Neonatal morbidities of prenatal and perinatal origin. In: Lockwood CJ, Copel JA, Dugoff L, et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2023:chap 73.
Johnston MV. Encephalopathies. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 616.
Kudva A, Abraham ME, Gold J, et al. Intrathecal baclofen, selective dorsal rhizotomy, and extracorporeal shockwave therapy for the treatment of spasticity in cerebral palsy: a systematic review. Neurosurg Rev. 2021;44(6):3209-3228.
Sidhu R, O'Banion DD, Hall C. Autism and other neurodevelopmental disabilities. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley's and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 90.
Smith SE, Gannotti M, Hurvitz EA, et al. Adults with cerebral palsy require ongoing neurologic care: a systematic review. Ann Neurol. 2021;89(5):860-871. PMID: 33550625 pubmed.ncbi.nlm.nih.gov/33550625/.
Review Date: 8/28/2023
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.