Neurosarcoidosis
Sarcoidosis - nervous system
Neurosarcoidosis is a form of sarcoidosis, in which inflammation occurs in the brain, spinal cord, and other areas of the nervous system.
Causes
Sarcoidosis is a chronic disease that affects many parts of the body, mostly the lungs. In a small number of people, the disease involves some part of the nervous system. This is called neurosarcoidosis.
Neurosarcoidosis may affect any part of the nervous system. Sudden facial weakness (facial palsy or facial droop) is a common neurological symptom that involves the nerves to the muscles of the face. Any other nerve in the skull can be affected, including those in the eye and those that control taste, smell, or hearing.
The spinal cord is another part of the nervous system that sarcoidosis can affect. People may have weakness in their arms and legs, and difficulty walking or controlling their urine or bowels. In some cases, the spinal cord is so severely affected that both legs are paralyzed.
The condition can also affect the parts of the brain involved in regulating many bodily functions, such as temperature, sleep, and stress responses. Other areas of the brain, including the pituitary gland at the base of the brain, can be affected.
Involvement of muscles or peripheral nerves can cause weakness and sensory loss.
Symptoms
The symptoms vary. Any part of the nervous system can be affected. Involvement of the brain or cranial nerves can cause:
- Confusion, disorientation
- Decreased hearing
- Dementia
- Dizziness, vertigo, or abnormal sensations of movement
- Double vision or other vision problems, including blindness
- Facial palsy (weakness, drooping)
- Headache
- Loss of sense of smell
- Loss of sense of taste, abnormal tastes
- Mental disturbances
- Seizures
- Speech impairment
Involvement of the pituitary gland can cause:
- Changes in menstrual periods
- Excessive tiredness or fatigue
- Excessive thirst
- High urine output
- Weight changes
- Hair changes
Involvement of one or more peripheral nerves can lead to:
- Abnormal sensations in any body part
- Loss of movement of any body part
- Loss of sensation in any body part
- Weakness of any body part
Exams and Tests
A neurological exam may show problems with one or more nerves.
A history of sarcoidosis followed by nerve-related symptoms highly suggests neurosarcoidosis. However, symptoms of the condition can mimic other medical disorders, including diabetes insipidus, hypopituitarism, multiple scleriosis, optic neuritis, meningitis, and certain tumors. Sometimes, the nervous system can be affected before a person is known to have sarcoidosis, or without affecting the lungs or other organs at all.
Blood tests are not very helpful in diagnosing the condition. A lumbar puncture may show signs of inflammation. Increased levels of angiotensin-converting enzyme may be found in the blood or cerebrospinal fluid (CSF). However, this is not a reliable diagnostic test.
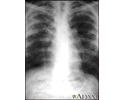
MRI of the brain and spinal cord may be helpful. A chest x-ray often reveals signs of sarcoidosis of the lungs. A biopsy of the affected tissue confirms the disorder. A biopsy of lymph nodes or other organs can show findings to support the diagnosis and to exclude other conditions. Sometimes a nerve or brain biopsy is needed.
Treatment
There is no known cure for sarcoidosis. Treatment is given if symptoms are severe or are getting worse. The goal of treatment is to reduce symptoms.
Corticosteroids such as prednisone are prescribed to reduce inflammation. They are often prescribed until symptoms get better or go away. You may need to take the medicines for months, or even years.
Other medicines may include hormone replacement and medicines that suppress the immune system.
If you have numbness, weakness, vision or hearing problems, or other problems due to damage of the nerves in the brain and spinal cord, you may need physical therapy, braces, a cane, walker, or wheelchair.
Mental disorders or dementia may require medicines for depression, safety interventions, and assistance with care.
Outlook (Prognosis)
Some cases go away on their own in 4 to 6 months. Others continue off and on for the rest of the person's life. Neurosarcoidosis can cause permanent disability and, in some cases, death.
Possible Complications
Complications vary, depending on which part of the nervous system is involved and how you respond to treatment. Slowly worsening or permanent loss of neurological function is possible. In rare cases, the brainstem may be involved. This is life threatening.
When to Contact a Medical Professional
Contact your health care provider if you have sarcoidosis and any neurological symptoms occur.
Go to the emergency room or call 911 or the local emergency number if you have a sudden loss of sensation, movement, or body function.
Prevention
Aggressive treatment of sarcoidosis turns off the body's faulty immune response before your nerves become damaged. This may reduce the chance that neurological symptoms will occur.
References
Iannuzzi MC. Sarcoidosis. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 89.
Josephson SA, Aminoff MJ. Neurological complications of systemic disease: adults. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 58.
Murphy OC, Krumholz A, Stern BJ. Sarcoidosis of the nervous system. In: Aminoff MJ, Josephson SA, eds. Aminoff's Neurology and General Medicine. 6th ed. Waltham, MA: Elsevier Academic Press; 2021:chap 49.
National Heart, Lung, and Blood Institute website. Sarcoidosis. www.nhlbi.nih.gov/health/sarcoidosis. Updated March 24, 2022. Accessed February 9, 2023.
Sarcoid, stage I - chest X-ray - illustration
Sarcoid, stage I - chest X-ray
illustration
Sarcoid, stage II - chest X-ray - illustration
Sarcoid, stage II - chest X-ray
illustration
Sarcoid, stage IV - chest x-ray - illustration
Sarcoid, stage IV - chest x-ray
illustration
Review Date: 1/23/2023
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School of Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.