Tuberous sclerosis
Bourneville disease
Tuberous sclerosis is a genetic disorder that affects the skin, brain/nervous system, kidneys, heart, and lungs. The condition can also cause tumors to grow in the brain. These tumors have a tuber or root-shaped appearance.
Causes
Tuberous sclerosis is genetic condition. Changes (mutations) in one of two genes, TSC1 and TSC2, are responsible for most cases.
Only one parent needs to pass on the mutation for the child to get the disease. However, two-thirds of cases are due to new mutations. In most cases, there is no family history of tuberous sclerosis.
This condition is one of a group of diseases called neurocutaneous syndromes. Both the skin and central nervous system (brain and spinal cord) are involved.
There are no known risk factors, other than having a parent with tuberous sclerosis. In that case, each child has a 50% chance of inheriting the disease.
Symptoms
Skin symptoms include:
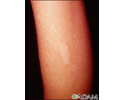
- Areas of the skin that are white (due to decreased pigment) and have either an ash leaf or confetti appearance
- Red patches on the face containing many blood vessels (facial angiofibromas)
- Raised patches of skin with an orange-peel texture (shagreen spots), often on the back
Brain symptoms include:
- Autism spectrum disorders
- Developmental delays
- Intellectual disability
- Seizures
Other symptoms include:
- Pitted tooth enamel.
- Rough growths under or around the fingernails and toenails.
- Rubbery noncancerous tumors on or around the tongue.
- Lung disease known as LAM (lymphangioleiomyomatosis). This is more common in women. In many cases, there are no symptoms. In other people, this can lead to shortness of breath, coughing blood, and lung collapse.
The symptoms vary from person to person. Some people have normal intelligence and no seizures. Others have intellectual disabilities or difficult-to-control seizures.
Exams and Tests
Signs may include:
- Abnormal heart rhythm (arrhythmia)
- Calcium deposits in the brain
- Noncancerous tumors in the brain
- Rubbery growths on the tongue or gums
- Tumor-like growth (hamartoma) on the retina, pale patches in the eye
- Tumors in the kidneys
Tests may include:
- CT scan of the head
- Chest CT
- Echocardiogram (ultrasound of the heart)
- MRI of the head
- Ultrasound of the kidney
- Ultraviolet light examination of the skin
DNA testing for the two genes that can cause this disease (TSC1 or TSC2) is available.
Regular ultrasound checks of the kidneys are important to make sure there is no tumor growth.
Treatment
There is no known cure for tuberous sclerosis. Because the disease can differ from person to person, treatment is based on the symptoms.
- Depending on the severity of the intellectual disability, the child may need special education.
- Some seizures are controlled with medicine (vigabatrin is first line for infantile spasms). Other children may need surgery.
- Small growths on the face (facial angiofibromas) may be removed by laser treatment. These growths tend to come back, and repeat treatments will be needed.
- Cardiac rhabdomyomas commonly disappear after puberty. Surgery to remove them is usually not needed.
- Brain tumors can be treated with medicines called mTOR inhibitors (sirolimus, everolimus).
- Kidney tumors are treated with surgery, or by reducing the blood supply using special x-ray techniques. mTOR inhibitors are being studied as another treatment for kidney tumors.
Support Groups
For additional information and resources, contact the Tuberous Sclerosis Alliance at www.tsalliance.org.
Outlook (Prognosis)
Children with mild tuberous sclerosis most often do well. However, children with severe intellectual disability or uncontrollable seizures often need lifelong assistance.
Sometimes when a child is born with severe tuberous sclerosis, one of the parents is found to have had a mild case of tuberous sclerosis that was not diagnosed.
The tumors in this disease tend to be noncancerous (benign). However, some tumors (such as kidney or brain tumors) can become cancerous.
Possible Complications
Complications may include:
- Brain tumors (astrocytoma)
- Heart tumors (rhabdomyoma)
- Severe intellectual disability
- Uncontrollable seizures
When to Contact a Medical Professional
Contact your health care provider if:
- Either side of your family has a history of tuberous sclerosis
- You notice symptoms of tuberous sclerosis in your child
Contact a genetic specialist if your child is diagnosed with cardiac rhabdomyoma. Tuberous sclerosis is the leading cause of this tumor.
Prevention
Genetic counseling is recommended for couples who have a family history of tuberous sclerosis and who want to have children.
Prenatal diagnosis is available for families with a known gene mutation or history of this condition. However, tuberous sclerosis often appears as a new DNA mutation. These cases are not preventable.
References
National Institute of Neurological Disorders and Stroke website. Tuberous sclerosis complex. www.ninds.nih.gov/health-information/disorders/tuberous-sclerosis-complex. Reviewed July 19, 2024. Accessed September 6, 2024.
Northrup H, Koenig MK, Pearson DA, et al. Tuberous sclerosis complex. GeneReviews. Seattle (WA): University of Washington, Seattle; July 13, 1999. Updated April 16, 2020. PMID: 20301399 pubmed.ncbi.nlm.nih.gov/20301399/.
Safier RA, Cleves-Bavon C, Gaesser J. Neurology. In: Zitelli BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 16.
Sahin M, Ullrich N, Srivastava S, Pinto A. Neurocutaneous syndromes. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 614.
Tsao H, Luo S. Neurofibromatosis and tuberous sclerosis complex. In: Bolognia JL, Schaffer JV, Cerroni L, et al, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 61.
Tuberous sclerosis, angiofibromas - face - illustration
Tuberous sclerosis, angiofibromas - face
illustration
Tuberous sclerosis - hypopigmented macule - illustration
Tuberous sclerosis - hypopigmented macule
illustration
Review Date: 7/26/2022
Reviewed By: Anna C. Edens Hurst, MD, MS, Associate Professor in Medical Genetics, The University of Alabama at Birmingham, Birmingham, AL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.