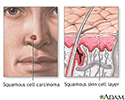
Squamous cell skin cancer
Cancer - skin - squamous cell; Skin cancer - squamous cell; Nonmelanoma skin cancer - squamous cell; NMSC - squamous cell; Squamous cell skin cancer; Squamous cell carcinoma of the skin
Squamous cell skin cancer is the second most common type of cancer in the United States.
Other common types of skin cancer are:
Causes
Squamous cell skin cancer affects the epidermis, the top layer of skin.
Squamous cell cancer may occur in undamaged skin. It can also occur in skin that has been injured or inflamed. Most squamous cell cancers occur on skin that is regularly exposed to sunlight or other ultraviolet radiation.
The earliest form of squamous cell cancer is called Bowen disease (or squamous cell carcinoma in situ). This type does not spread to nearby tissues, because it is still in the outermost layer of the skin.
Actinic keratosis is a precancerous skin lesion that may become a squamous cell cancer. (A lesion is a problem area of the skin.)
A keratoacanthoma is a mild type of squamous cell cancer that grows rapidly.
Risks of squamous cell cancer include:
- Having light-colored skin, blue or green eyes, or blond or red hair.
- Long-term, daily sun exposure (such as in people who work outside).
- Many severe sunburns early in life.
- Older age.
- Having had many x-rays.
- Chemical exposure, such as arsenic.
- A weakened immune system, especially in people who have had an organ transplant.
Symptoms
Squamous cell cancer usually occurs on the face, ears, neck, hands, or arms. It may occur in other areas.
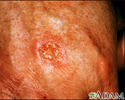
The main symptom is a growing bump that may have a rough, scaly surface and flat reddish patches.
The earliest form (squamous cell carcinoma in situ) can appear as a scaly, crusted, and large reddish patch that can be larger than 1 inch (2.5 centimeters).
A sore that does not heal can be a sign of squamous cell cancer. Any change in an existing wart, mole, or other skin lesion could be a sign of skin cancer.
Exams and Tests
Your health care provider will check your skin and look at the size, shape, color, and texture of any suspicious areas.
If your provider thinks you might have skin cancer, a piece of skin will be removed. This is called a skin biopsy. The sample is sent to a lab for examination under a microscope.
A skin biopsy must be done to confirm squamous cell skin cancer or other skin cancers.
Treatment
Treatment depends on the size and location of the skin cancer, how far it has spread, and your overall health. Some squamous cell skin cancers may be more difficult to treat.
Treatment may involve:
- Excision: Cutting out the skin cancer and stitching the skin together.
- Curettage and electrodessication: Scraping away cancer cells and using electricity to kill any that remain. It is used to treat cancers that are not very large or deep.
- Cryosurgery: Freezing the cancer cells, which kills them. This is used for small and superficial (not very deep) cancers.
- Medicines: Skin creams containing imiquimod or 5-fluorouracil for superficial squamous cell cancer.
- Mohs surgery: Removing a layer of skin and looking at it immediately under a microscope, then removing layers of skin until there are no signs of the cancer, usually used for skin cancers on the nose, ears, and other areas of the face.
- Photodynamic therapy: Treatment using light may be used to treat superficial cancers.
- Radiation therapy: may be used if squamous cell cancer has spread to organs or lymph nodes or if the cancer cannot be treated with surgery.
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
How well a person does depends on many things, including how soon the cancer was diagnosed, the location, and whether or not you have a weakened immune system. Most of these cancers are cured when treated early.
Some squamous cell cancers may return. There is also a risk that squamous cell skin cancer may spread to other parts of the body.
When to Contact a Medical Professional
Contact your provider for an appointment if you have a sore or spot on your skin that changes in:
- Appearance
- Color
- Size
- Texture
Also contact your provider if a spot becomes painful or swollen or if it starts to bleed or itch.
Prevention
Experts disagree about the value of routine skin examinations by your provider. But all agree it's important to know your own skin and to contact your provider if you notice anything unusual.
The best way to prevent skin cancer is to reduce your exposure to sunlight. Always use sunscreen:
- Apply sunscreen with sun protection factor (SPF) of at least 30, even when you are going outdoors for a short time.
- Apply a large amount of sunscreen on all exposed areas, including ears and feet.
- Look for sunscreen that blocks both UVA and UVB light.
- Use a water-resistant sunscreen.
- Apply sunscreen at least 30 minutes before going out. Follow package instructions about how often to reapply. Be sure to reapply after swimming or sweating.
- Use sunscreen in winter and on cloudy days too.
Other measures to help you avoid too much sun exposure:
- Ultraviolet light is most intense between 10 a.m. and 4 p.m. So try to avoid the sun during these hours.
- Protect your skin by wearing wide-brim hats, long-sleeve shirts, long skirts, or pants. You can also buy sun-protective clothing.
- Avoid surfaces that reflect light more, such as water, sand, concrete, and areas that are painted white.
- The higher the altitude, the faster your skin burns.
- Do not use sun lamps and tanning beds (salons). Spending 15 to 20 minutes at a tanning salon is as dangerous as a day spent in the sun.
References
American Cancer Society website. Skin cancer prevention and early detection. www.cancer.org/content/dam/CRC/PDF/Public/6930.00.pdf. Reviewed April 20, 2017. Accessed October 3, 2023.
Dinulos JGH. Premalignant and malignant nonmelanoma skin tumors. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 21.
National Cancer Institute website. Skin cancer treatment (PDQ) - Health Professional Version. www.cancer.gov/types/skin/hp/skin-treatment-pdq#section/_222. Updated March 2, 2023. Accessed July 17, 2023.
National Comprehensive Cancer Network website. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Squamous cell skin cancer. Version 1.2024 – November 9, 2023. www.nccn.org/professionals/physician_gls/pdf/squamous.pdf. Updated November 9, 2023. Accessed November 27, 2023.
US Preventive Services Task Force, Mangione CM, Barry MJ, et al. Screening for skin cancer: US Preventive Services Task Force recommendation statement. JAMA. 2023;329(15):1290-1295. PMID: 37071089 pubmed.ncbi.nlm.nih.gov/37071089/.
Squamous cell cancer - illustration
Squamous cell cancer
illustration
Sun protection - illustration
Sun protection
illustration
Bowen's disease on the hand - illustration
Bowen's disease on the hand
illustration
Keratoacanthoma - illustration
Keratoacanthoma
illustration
Keratoacanthoma - illustration
Keratoacanthoma
illustration
Skin cancer, squamous cell - close-up - illustration
Skin cancer, squamous cell - close-up
illustration
Skin cancer - squamous cell on the hands - illustration
Skin cancer - squamous cell on the hands
illustration
Squamous cell carcinoma - invasive - illustration
Squamous cell carcinoma - invasive
illustration
Cheilitis - actinic - illustration
Cheilitis - actinic
illustration
Review Date: 7/1/2023