Endometrial cancer
Endometrial adenocarcinoma; Uterine adenocarcinoma; Uterine cancer; Adenocarcinoma - endometrium; Adenocarcinoma - uterus; Cancer - uterine; Cancer - endometrial; Uterine corpus cancer
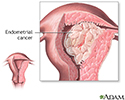
Endometrial cancer is cancer that starts in the endometrium, the lining of the uterus (womb).
Causes
Endometrial cancer is the most common type of uterine cancer. The exact cause of endometrial cancer is not known. An increased level of estrogen hormone may play a role. This stimulates the buildup of the lining of the uterus. This can lead to abnormal overgrowth of the endometrium and cancer.
Most cases of endometrial cancer occur between the ages of 60 and 70. A few cases may occur before age 40.
The following factors related to your hormones increase your risk for endometrial cancer:
- Estrogen replacement therapy without the use of progesterone
- History of endometrial polyps
- Infrequent periods
- Never being pregnant
- Obesity
- Diabetes
- Polycystic ovary syndrome (PCOS)
- Starting menstruation at an early age (before age 12)
- Starting menopause after age 50
- Tamoxifen, a drug used for breast cancer treatment
Women with the following conditions also seem to be at a higher risk for endometrial cancer:
- Colon or breast cancer
- Gallbladder disease
- High blood pressure
Symptoms
Symptoms of endometrial cancer include:
- Abnormal bleeding from the vagina, including bleeding between periods or spotting/bleeding after menopause
- Extremely long, heavy, or frequent episodes of vaginal bleeding after age 40
- Lower abdominal pain or pelvic cramping
Exams and Tests
During the early stages of disease, a pelvic exam is often normal.
- In advanced stages, there may be changes in the size, shape, or feel of the uterus or surrounding structures.
- Pap smear (may raise a suspicion for endometrial cancer, but does not diagnose it)
Based on your symptoms and other findings, other tests may be needed. Some can be done in your health care provider's office. Others may be done at a hospital or surgical center:
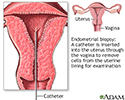
- Endometrial biopsy: Using a small or thin catheter (tube), tissue is taken from the lining of the uterus (endometrium). The cells are examined under a microscope to see if any appear to be abnormal or cancerous.
- Hysteroscopy: A thin telescope-like device is inserted through the vagina and the opening of the cervix. It lets the provider view the inside of the uterus. Tissue can also be removed for analysis during the exam.
- Ultrasound: Sound waves are used to make a picture of the pelvic organs. The ultrasound may be performed abdominally or vaginally. An ultrasound can determine if the lining of the uterus appears abnormal or thickened.
- Sonohysterography: Fluid is placed in the uterus through a thin tube, while vaginal ultrasound images are made of the uterus. This procedure can be done to determine the presence of any abnormal uterine mass which may be an indication of cancer.
- Magnetic resonance imaging (MRI): In this imaging test, powerful magnets are used to create images of internal organs.
If cancer is found, imaging tests may be done to see if the cancer has spread to other parts of the body. This is called staging.
Stages of endometrial cancer are:
- Stage 1: The cancer is only in the uterus.
- Stage 2: The cancer is in the uterus and cervix.
- Stage 3: The cancer has spread outside of the uterus, but not beyond the true pelvis area. Cancer may involve the lymph nodes in the pelvis or near the aorta (the major artery in the abdomen).
- Stage 4: The cancer has spread to the inner surface of the bowel, bladder, abdomen, or other organs.
Cancer is also described as grade 1, 2, or 3. Grade 1 is the least aggressive, and grade 3 is the most aggressive. Aggressive means that the cancer grows and spreads quickly.
Treatment
Treatment options include:
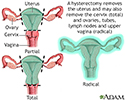
Surgery to remove the uterus (hysterectomy) may be done in women with early stage 1 cancer. The surgeon may also remove the tubes and ovaries.
Surgery combined with radiation therapy is another treatment option. It is often used for women with:
- Stage 1 disease that has a high chance of returning, has spread to the lymph nodes, or is a grade 2 or 3
- Stage 2 disease
Chemotherapy or hormonal therapy may be considered in some cases, most often for those with stage 3 and 4 disease.
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
Endometrial cancer is usually diagnosed at an early stage.
If the cancer has not spread, 95% of women are alive 5 years after treatment. If the cancer has spread to distant organs, about 25% of women are still alive after 5 years.
Possible Complications
Complications may include any of the following:
- Anemia due to blood loss (before diagnosis)
- Perforation (hole) of the uterus, which may occur during a dilation and curettage (D and C) or endometrial biopsy
- Problems from surgery, radiation, and chemotherapy
When to Contact a Medical Professional
Contact your provider for an appointment if you have any of the following:
- Any bleeding or spotting that occurs after the onset of menopause
- Bleeding or spotting after intercourse or douching
- Bleeding lasting longer than 7 days
- Irregular menstrual cycles that occur twice per month
- New discharge after menopause has begun
- Pelvic pain or cramping that does not go away
Prevention
There is no effective screening test for endometrial cancer.
Women with risk factors for endometrial cancer should be followed closely by their providers. This includes women who are taking:
- Estrogen replacement therapy without progesterone therapy
- Tamoxifen for more than 2 years
Frequent pelvic exams, Pap smears, vaginal ultrasounds, and endometrial biopsy may be considered in some cases.
The risk for endometrial cancer is reduced by:
- Maintaining a normal weight
- Using birth control pills for over a year
References
Armstrong DK. Gynecologic cancers. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 184.
Boggess JF, Kilgore JE, Tran A-Q. Uterine cancer. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 85.
Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E. Endometrial cancer. Lancet. 2016;387(10023):1094-1108. PMID: 26354523 pubmed.ncbi.nlm.nih.gov/26354523/.
National Cancer Institute website. Endometrial cancer treatment (PDQ)-health professional version. www.cancer.gov/types/uterine/hp/endometrial-treatment-pdq. Updated February 8, 2024. Accessed May 30, 2024.
National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology (NCCN Guidelines): uterine neoplasms. Version 2.2024. www.nccn.org/professionals/physician_gls/pdf/uterine.pdf. Updated March 6, 2024. Accessed May 30, 2024.
Hysterectomy
Animation
Pelvic laparoscopy - illustration
Pelvic laparoscopy
illustration
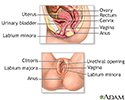
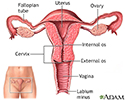
Female reproductive anatomy - illustration
Female reproductive anatomy
illustration
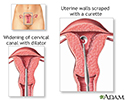
D and C - illustration
D and C
illustration
Endometrial biopsy - illustration
Endometrial biopsy
illustration
Hysterectomy - illustration
Hysterectomy
illustration
Uterus - illustration
Uterus
illustration
Endometrial cancer - illustration
Endometrial cancer
illustration
Pelvic laparoscopy - illustration
Pelvic laparoscopy
illustration
Female reproductive anatomy - illustration
Female reproductive anatomy
illustration
D and C - illustration
D and C
illustration
Endometrial biopsy - illustration
Endometrial biopsy
illustration
Hysterectomy - illustration
Hysterectomy
illustration
Uterus - illustration
Uterus
illustration
Endometrial cancer - illustration
Endometrial cancer
illustration
Review Date: 3/31/2024
Reviewed By: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.