Colitis
Colitis is swelling (inflammation) of the large intestine (colon).
Most of the time, the cause of colitis is not known.
Causes of colitis include:
- Infections caused by a virus or a parasite
- Food poisoning due to bacteria
- Crohn disease
- Ulcerative colitis
- Lack of blood flow to the colon (ischemic colitis)
- Past radiation to the colon (radiation colitis and strictures)
- Necrotizing enterocolitis in newborns
- Pseudomembranous colitis caused by Clostridium difficile infection (now called Clostridiodes difficile)
Symptoms
Symptoms can include:
- Abdominal pain and bloating that may be constant or come and go
- Bloody stools
- Constant urge to have a bowel movement (tenesmus)
- Dehydration
- Diarrhea
- Fever
Exams and Tests
The health care provider will perform a physical exam. You will also be asked questions about your symptoms, such as:
- How long have you had the symptoms?
- How severe is your pain?
- How often do you have pain and how long does it last?
- How often do you have diarrhea?
- Have you traveled recently?
- Have you taken antibiotics recently?
Your provider may recommend a flexible sigmoidoscopy or colonoscopy. During this test, a flexible tube is inserted through your rectum to examine your colon. You may have biopsies taken during this exam. Biopsies may show changes related to inflammation. This can help determine the cause of colitis.
Other studies that can identify colitis include:
- CT scan of the abdomen
- MRI of the abdomen
- Barium enema
- Stool culture
- Stool examination for ova and parasites
Treatment
Your treatment will depend on the cause of the disease.
Outlook (Prognosis)
The outlook depends on the cause of the problem.
- Crohn disease is a chronic condition which has no cure but can be controlled. Biologic agents are very effective in controlling symptoms of Crohn colitis.
- Ulcerative colitis can usually be controlled with medicines. If not controlled, it can be cured by surgically removing the colon.
- Viral, bacterial, and parasitic colitis can be cured with appropriate medicines.
- Pseudomembranous colitis can usually be cured with appropriate antibiotics.
Possible Complications
Complications may include:
- Bleeding with bowel movements
- Perforation of the colon
- Toxic megacolon
- Sore (ulceration)
When to Contact a Medical Professional
Contact your provider if you have symptoms such as:
- Abdominal pain that does not get better
- Blood in the stool or stools that look black
- Diarrhea or vomiting that does not go away
- Swollen abdomen
References
Ananthakrishnan AN, Regueiro MD. Management of inflammatory bowel diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 116.
Lichtenstein GR. Inflammatory bowel disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 127.
Pardi DS, Cotter TG. Other diseases of the colon. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 128.
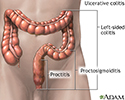
Ulcerative colitis - illustration
Ulcerative colitis
illustration
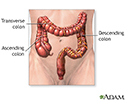
Large intestine (colon) - illustration
Large intestine (colon)
illustration
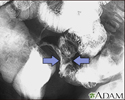
Crohn disease - X-ray - illustration
Crohn disease - X-ray
illustration
Inflammatory bowel disease - illustration
Inflammatory bowel disease
illustration
Large intestine - illustration
Large intestine
illustration
Ulcerative colitis - illustration
Ulcerative colitis
illustration
Large intestine (colon) - illustration
Large intestine (colon)
illustration
Crohn disease - X-ray - illustration
Crohn disease - X-ray
illustration
Inflammatory bowel disease - illustration
Inflammatory bowel disease
illustration
Large intestine - illustration
Large intestine
illustration
Review Date: 8/7/2023
Reviewed By: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.