Orchitis
Epididymo - orchitis; Testis infection
Orchitis is swelling (inflammation) of one or both of the testicles.
Causes
Orchitis may be caused by an infection. Many types of bacteria and viruses can cause this condition.
The most common virus that causes orchitis is mumps. It most often occurs in boys after puberty. Orchitis most often develops 4 to 6 days after the mumps begins.
Orchitis may also occur along with infections of the prostate or epididymis.
Orchitis may be caused by a sexually transmitted infection (STI), such as gonorrhea or chlamydia. The rate of sexually transmitted orchitis or epididymitis is higher in men ages 19 to 35.
Risk factors for sexually transmitted orchitis include:
- High-risk sexual behaviors
- Multiple sexual partners
- Personal history of gonorrhea or another STI
- Sexual partner with a diagnosed STI
Risk factors for orchitis not due to an STI include:
- Being older than age 45
- Long-term use of a Foley catheter
- Not being vaccinated against the mumps virus
- Problems of the urinary tract that were present at birth (congenital)
- Repeated urinary tract infections
- Surgery of the urinary tract (genitourinary surgery)
- BPH (benign prostatic hyperplasia) - enlarged prostate
- Urethral stricture (scarring inside urinary tract that causes narrowing of the passageway)
Symptoms
Symptoms include:
- Pain in the testicle
- Blood in the semen
- Discharge from penis
- Fever
- Groin pain
- Pain with intercourse or ejaculation
- Pain with urination (dysuria)
- Scrotal swelling
- Tender, swollen groin area on affected side
- Tender, swollen, heavy feeling in the testicle
Exams and Tests
A physical exam may show:
- Enlarged or tender prostate gland
- Tender and enlarged lymph nodes in the groin (inguinal) area on the affected side
- Tender and enlarged testicle on the affected side
- Redness or tenderness of scrotum
Tests may include:
- Complete blood count (CBC)
- Testicular ultrasound
- Tests to screen for chlamydia and gonorrhea (urethral smear)
- Urinalysis
- Urine culture (clean catch) -- may need several samples, including initial stream, midstream, and after prostate massage
Treatment
Treatment may include:
- Antibiotics, if the infection is caused by bacteria. (In the case of gonorrhea or chlamydia, sexual partners must also be treated.)
- Anti-inflammatory medicines.
- Pain medicines.
- Bed rest with the scrotum elevated and ice packs applied to the area.
Outlook (Prognosis)
Getting the right diagnosis and treatment for orchitis caused by bacteria can most often allow the testicle to recover normally.
You will need further testing to rule out testicular cancer if the testicle does not completely return to normal after treatment.
Mumps orchitis has no effective treatment, and the outcome can vary. Men who have had mumps orchitis can become sterile.
Possible Complications
Some boys who get orchitis caused by mumps will have shrinking of the testicles (testicular atrophy).
Orchitis may also cause infertility.
Other potential complications include:
- Chronic epididymitis
- Death of testicle tissue (testicular infarction)
- Fistula on the skin of the scrotum (cutaneous scrotal fistula)
- Scrotal abscess
Acute pain in the scrotum or testicles can be caused by twisting of the testicular blood vessels (torsion). This is a medical emergency that requires immediate surgery.
A swollen testicle with little or no pain may be a sign of testicular cancer. If this is the case, you should have a testicular ultrasound.
When to Contact a Medical Professional
See your health care provider for an exam if you have testicle problems.
Get emergency medical help if you have sudden pain in the testicle.
Prevention
Things you can do to prevent the problem include:
- Get vaccinated against mumps.
- Practice safer sex behaviors to decrease your risk for STIs.
References
Mason WH, Gans HA. Mumps. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 275.
McGowan CC. Prostatitis, epididymitis, and orchitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 110.
Pontari M. Inflammatory and pain conditions of the male genitourinary tract: prostatitis and related pain conditions, orchitis, and epididymitis. In: Partin AW, Domochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 56.
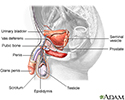
Male reproductive anatomy - illustration
Male reproductive anatomy
illustration
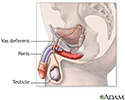
Male reproductive system - illustration
Male reproductive system
illustration
Review Date: 1/1/2023
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.