Epidural hematoma
Extradural hematoma; Extradural hemorrhage; Epidural hemorrhage; EDH
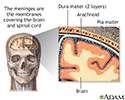
An epidural hematoma (EDH) is bleeding between the inside of the skull and the outer covering of the brain (called the dura mater).
Causes
An EDH is often caused by a skull fracture during childhood or adolescence. The membrane covering the brain is not as closely attached to the skull as it is in older people and children younger than 2 years. Therefore, this type of bleeding is more common in young people.
An EDH can also occur due to rupture of a blood vessel, usually an artery. The blood vessel then bleeds into the space between the dura and the skull.
The affected vessels are often torn by skull fractures. The fractures are most often the result of a severe head injury, such as those caused by motorcycle, bicycle, skateboard, snow boarding, or automobile accidents.
Rapid bleeding causes a collection of blood (hematoma) that presses on the brain. The pressure inside the head (intracranial pressure, ICP) increases quickly. This pressure may result in more brain injury.
Symptoms
Contact a health care provider for any head injury that results in even a brief loss of consciousness, or if there are any other symptoms after a head injury (even without loss of consciousness).
The typical pattern of symptoms that indicate an EDH is a loss of consciousness, followed by alertness, then loss of consciousness again. But this pattern may NOT appear in all people.
The most important symptoms of an EDH are:
- Confusion
- Dizziness
- Drowsiness or altered level of alertness
- Enlarged pupil in one eye
- Headache (severe)
- Head injury or trauma followed by loss of consciousness, a period of alertness, then rapid deterioration back to unconsciousness
- Nausea or vomiting
- Weakness in part of the body, usually on the opposite side from the side with the enlarged pupil
- Seizures can occur as a result of head impact
The symptoms usually occur within minutes to hours after a head injury and indicate an emergency situation.
Sometimes, bleeding does not start for hours after a head injury. The symptoms of pressure on the brain also do not occur right away.
Exams and Tests
The brain and nervous system (neurological) examination may show that a specific part of the brain is not working well (for instance, there may be arm weakness on one side).
The exam may also show signs of increased ICP, such as:
- Headaches
- Somnolence
- Confusion
- Nausea and vomiting
If there is increased ICP, emergency surgery may be needed to relieve the pressure and prevent further brain injury.
A non-contrast head CT scan will confirm the diagnosis of EDH, and will pinpoint the exact location of the hematoma and any associated skull fracture. MRI may be useful to identify small epidural hematomas from subdural ones.
Treatment
An EDH is an emergency condition. Treatment goals include:
- Taking measures to save the person's life
- Controlling symptoms
- Minimizing or preventing permanent damage to the brain
Life support measures may be required. Emergency surgery is often necessary to reduce pressure within the brain. This may include drilling a small hole in the skull to relieve pressure and allow blood to drain outside the skull.
Large hematomas or solid blood clots may need to be removed through a larger opening in the skull (craniotomy).
Medicines used in addition to surgery will vary according to the type and severity of symptoms and brain damage that occurs.
Antiseizure medicines may be used to control or prevent seizures. Some medicines called hyperosmotic agents may be used to reduce brain swelling.
For people on blood thinners or with bleeding disorders, treatments to prevent further bleeding might be needed.
Outlook (Prognosis)
An EDH has a high risk of death without prompt surgical intervention. Even with prompt medical attention, a significant risk of death and disability remains.
Possible Complications
There is a risk of permanent brain injury, even if EDH is treated quickly. Symptoms (such as seizures) may persist for several months, even after treatment. In time they may become less frequent or disappear. Seizures may begin up to 2 years after the injury.
In adults, most recovery occurs in the first 6 months. Usually there is some improvement over 2 years.
If there is brain damage, full recovery isn't likely. Other complications include permanent symptoms, such as:
- Herniation of the brain and permanent coma
- Normal pressure hydrocephalus, which can lead to weakness, headaches, incontinence, and difficulty walking
- Paralysis or loss of sensation (which began at the time of the injury)
When to Contact a Medical Professional
Go to the emergency room or call 911 or the local emergency number if symptoms of EDH occur.
Spinal injuries often occur with head injuries. If you must move the person before help arrives, try to keep his or her neck and spine still.
Contact your provider if these symptoms persist after treatment:
- Memory loss or problems focusing
- Dizziness
- Headache
- Anxiety
- Speech problems
- Loss of movement in part of the body
Go to the emergency room or call 911 or the local emergency number if these symptoms develop after treatment:
- Trouble breathing
- Seizures
- Enlarged pupils of the eyes or the pupils are not same size
- Decreased responsiveness
- Loss of consciousness
Prevention
An EDH may not be preventable once a head injury has occurred.
To lessen the risk of head injury, use the right safety equipment (such as hard hats, bicycle or motorcycle helmets, and seat belts).
Follow safety precautions at work and in sports and recreation. For example, do not dive into water if the water depth is unknown or if rocks may be present.
References
National Institute of Neurological Disorders and Stroke website. Traumatic brain injury. www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi. Updated July 19, 2024. Accessed September 6, 2024.
Shahlaie K, Menon DK, Hawryluk GWJ. Clinical pathophysiology of traumatic brain injury. In: Winn HR, ed. Youmans and Winn Neurological Surgery. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 384.
Wermers JD, Hutchison LH. Trauma. In: Coley BD, ed. Caffey's Pediatric Diagnostic Imaging. 13th ed. Philadelphia, PA: Elsevier; 2019:chap 39.
Review Date: 7/26/2022
Reviewed By: Evelyn O. Berman, MD, Assistant Professor of Neurology and Pediatrics at University of Rochester, Rochester, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 09/06/2024.