Uterine prolapse
Pelvic relaxation - uterine prolapse; Pelvic floor hernia; Prolapsed uterus; Incontinence - prolapse
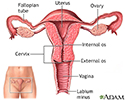
Uterine prolapse occurs when the womb (uterus) drops down and presses into the vaginal area.
Causes
Muscles, ligaments, and other structures hold the uterus in the pelvis. If these tissues are weak or stretched, the uterus drops into the vaginal canal. This is called prolapse.
This condition is more common in women who have had 1 or more vaginal births.
Other things that can cause or lead to uterine prolapse include:
- Normal aging
- Lack of estrogen after menopause
- Conditions that put pressure on the pelvic muscles, such as chronic cough and obesity
- Pelvic tumor (rare)
Repeated straining to have a bowel movement due to long-term constipation can make the problem worse.
Symptoms
Symptoms may include:
- Pressure or heaviness in the pelvis or vagina
- Problems with sexual intercourse
- Leaking urine or sudden urge to empty the bladder
- Low backache
- Uterus and cervix that bulge into the vaginal opening
- Repeated bladder infections
- Vaginal bleeding
- Increased vaginal discharge
Symptoms may be worse when you stand or sit for a long time. Exercise or lifting may also make symptoms worse.
Exams and Tests
Your health care provider will do a pelvic exam. You will be asked to bear down as if you are trying to push out a baby. This shows how far your uterus has dropped.
- Uterine prolapse is mild when the cervix drops into the lower part of the vagina.
- Uterine prolapse is moderate when the cervix drops out of the vaginal opening.
Other things the pelvic exam may show are:
- The bladder and front wall of the vagina are bulging into the vagina (cystocele).
- The rectum and back wall of the vagina (rectocele) are bulging into the vagina.
- The urethra and bladder are lower in the pelvis than usual.
Treatment
You do not need treatment unless you are bothered by the symptoms.
Many women will get treatment by the time the uterus drops to the opening of the vagina.
LIFESTYLE CHANGES
The following can help you control your symptoms:
- Lose weight if you are obese.
- Avoid heavy lifting or straining.
- Get treated for a chronic cough. If your cough is due to smoking, try to quit.
VAGINAL PESSARY
Your provider may recommend placing a rubber or plastic donut-shaped device, into your vagina. This is called a pessary. This device holds your uterus in place.
The pessary may be used for short-term or long-term. The device is fitted for your vagina. Some pessaries are similar to a diaphragm used for birth control.
Pessaries must be cleaned regularly. Sometimes they need to be cleaned by your provider. Many women can be taught how to insert, clean, and remove a pessary.
Side effects of pessaries include:
- Foul smelling discharge from the vagina
- Irritation of the lining of the vagina
- Ulcers in the vagina
- Problems with vaginal sexual intercourse
SURGERY
Surgery should not be done until the prolapse symptoms are worse than the risks of having surgery. The type of surgery will depend on:
- The severity of the prolapse
- The woman's plans for future pregnancies
- The woman's age, health, and other medical problems
- The woman's desire to retain vaginal function
There are some surgical procedures that can be done without removing the uterus, such as a sacrospinous fixation. This procedure involves using nearby ligaments to support the uterus. Other procedures are also available.
Often, a vaginal hysterectomy can be done at the same time as the procedure to correct uterine prolapse. Any sagging of the vaginal walls, urethra, bladder, or rectum can be surgically corrected at the same time.
Outlook (Prognosis)
Most women with mild uterine prolapse do not have symptoms that require treatment.
Vaginal pessaries can be effective for many women with uterine prolapse.
Surgery often provides very good results. However, some women may need to have the treatment again in the future.
Possible Complications
Ulceration and infection of the cervix and vaginal walls may occur in severe cases of uterine prolapse.
Urinary tract infections and other urinary symptoms may occur because of a cystocele. Constipation and hemorrhoids may occur because of a rectocele.
When to Contact a Medical Professional
Contact your provider if you have symptoms of uterine prolapse.
Prevention
Tightening the pelvic floor muscles using Kegel exercises helps to strengthen the muscles and reduces the risk of developing uterine prolapse.
Estrogen therapy after menopause may help with vaginal muscle tone.
References
Cox L, Rovner ES. Bladder and female urethral diverticula. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 130.
Guerrero K. Pelvic organ prolapse. In: Magowan BA, Owen P, Thomson A, eds. Clinical Obstetrics and Gynaecology. 5th ed. Philadelphia, PA: Elsevier; 2023:chap 10.
Kirby AC, Lentz GM. Pelvic organ prolapse, abdominal hernias, and inguinal hernias: diagnosis and management. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 20.
Newman DK, Burgio KL. Conservative management of urinary incontinence: behavioral and pelvic floor therapy and urethral and pelvic devices. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 80.
Winters JC, Krlin RM, Hallner B. Vaginal and abdominal reconstructive surgery for pelvic organ prolapse. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 124.
Review Date: 7/12/2023
Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.