Vaginal yeast infection
Yeast infection - vagina; Vaginal candidiasis; Monilial vaginitis
Vaginal yeast infection is an infection of the vagina. It is most often due to the fungus Candida albicans.
Causes
Most women have a vaginal yeast infection at some time. Candida albicans is a common type of fungus. It is often found in small amounts in the vagina, mouth, digestive tract, and on the skin. Most of the time, it does not cause infection or symptoms.
Candida and the many other germs that normally live in the vagina keep each other in balance. Sometimes the number of candida increases. This leads to a yeast infection.
This can happen if:
- You are taking antibiotics used to treat another infection. Antibiotics change the normal balance between germs in the vagina.
- You are pregnant
- You are obese
- You have diabetes
- You are taking medicines or have an illness that suppresses your immune system.
A yeast infection is not spread through sexual contact. However, some men may develop symptoms after having sexual contact with an infected partner. These symptoms may include itching, rash or irritation of the penis.
Having many vaginal yeast infections may be a sign of other health problems. Other vaginal infections and discharges can be mistaken for a vaginal yeast infection.
Symptoms
Symptoms include:
- Abnormal vaginal discharge. Discharge can range from slightly watery, white discharge to thick, white, and chunky (like cottage cheese).
- Itching and burning of the vagina and labia
- Pain with intercourse
- Painful urination
- Redness and swelling of the skin just outside of the vagina (vulva)
Exams and Tests
Your health care provider will do a pelvic exam. It may show:
- Swelling and redness of the skin of the vulva, in the vagina, and on the cervix
- Dry, white spots on the vaginal wall
- Cracks in the skin of the vulva
A small amount of the vaginal discharge may be examined using a microscope. This is called a wet mount and KOH test.
Sometimes, a culture is taken if:
- The infection does not get better with treatment
- The infection recurs
Your provider may order other tests to check for other causes of your symptoms.
Treatment
Medicines to treat vaginal yeast infections are available as creams, ointments, vaginal tablets or suppositories and oral tablets. Most can be bought without needing to see your provider. If you do need to see your provider, you may wish to ask them about the use of boric acid for yeast infections.
Treating yourself at home is probably OK if:
- Your symptoms are mild and you do not have pelvic pain or a fever
- This is not your first yeast infection and you have not had many yeast infections in the past
- You are not pregnant
- You are not worried about other sexually transmitted infections (STI) from recent sexual contact
Medicines you can buy yourself to treat a vaginal yeast infection are:
- Miconazole
- Clotrimazole
- Tioconazole
- Butoconazole
When using these medicines:
- Read the package inserts carefully and use them as directed.
- You will need to take the medicine for 1 to 7 days, depending on which medicine you buy. (If you do not get repeated infections, a 1-day medicine might work for you.)
- Do not stop using these medicines early because your symptoms are better.
Your provider can also prescribe a pill that you only take by mouth once.
If your symptoms are worse or you get vaginal yeast infections often, you may need:
- Medicine for up to 14 days
- Azole vaginal cream or fluconazole pill every week to prevent new infections
To help prevent and treat vaginal discharge:
- Keep your genital area clean and dry. Avoid soap and rinse with water only. Sitting in a warm, but not hot, bath may help your symptoms.
- Avoid douching. Although many women feel cleaner if they douche after their period or intercourse, it may worsen vaginal discharge. Douching removes healthy bacteria lining the vagina that protect against infection.
- Eat yogurt with live cultures or take Lactobacillus acidophilus tablets when you are on antibiotics. This may help to prevent a yeast infection.
- Use condoms to avoid catching or spreading other infections.
- Avoid using feminine hygiene sprays, fragrances, or powders in the genital area.
- Avoid wearing tight-fitting pants or shorts. These may cause irritation and sweating.
- Wear cotton underwear or cotton-crotch pantyhose. Avoid underwear made of silk or nylon. These can increase sweating in the genital area, which leads to growth of more yeast.
- Keep your blood sugar level under good control if you have diabetes.
- Avoid wearing wet bathing suits or exercise clothing for long periods of time. Wash sweaty or wet clothes after each use.
Outlook (Prognosis)
Most of the time, symptoms go away completely with proper treatment.
Possible Complications
A lot of scratching may cause the skin to crack, making you more likely to get a skin infection.
A woman may have diabetes or weak immune system (such as in HIV) if:
- The infection recurs right after treatment
- The yeast infection does not respond well to treatment
When to Contact a Medical Professional
Contact your provider if:
- This is the first time that you have had symptoms of a vaginal yeast infection.
- You are not sure if you have a yeast infection.
- Your symptoms don't go away after using over-the-counter medicines.
- Your symptoms get worse.
- You develop other symptoms.
- You may have been exposed to an STI.
References
Dinulos JGH. Superficial fungal infections. In: Dinulos JGH, ed. Habif's Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 13.
Eckert LO, Lentz GM. Genital tract infections: vulva, vagina, cervix, toxic shock syndrome, endometritis, and salpingitis. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 23.
Oquendo Del Toro HM, Hoefgen HR. Vulvovaginitis. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 564.
Pappas PG. Candidiasis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 310.
Candida - fluorescent stain - illustration
Candida - fluorescent stain
illustration
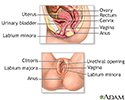
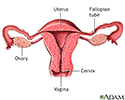
Female reproductive anatomy - illustration
Female reproductive anatomy
illustration
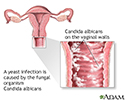
Yeast infections - illustration
Yeast infections
illustration
Secondary infection - illustration
Secondary infection
illustration
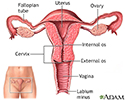
Uterus - illustration
Uterus
illustration
Normal uterine anatomy (cut section) - illustration
Normal uterine anatomy (cut section)
illustration
Review Date: 7/12/2023