Eyelid lift
Blepharoplasty; Ptosis repair - eyelid lift
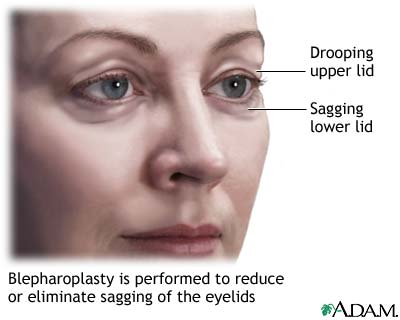
Eyelid lift surgery is done to repair sagging or drooping upper eyelids (ptosis) and remove excess skin from the eyelids. The surgery is called ptosis repair and blepharoplasty.
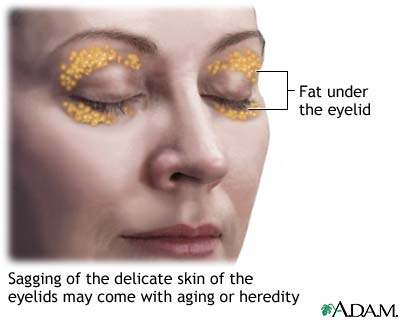
Sagging or drooping eyelids occur with increasing age. Some people are born with droopy eyelids or develop a disease that causes eyelid drooping.
Description
Eyelid surgery is done in a surgeon's office. Or, it is done as outpatient surgery in a surgery center.
The procedure is done as follows:
- You are given medicine to help you relax.
- The surgeon injects numbing medicine (anesthesia) around the eye so you do not feel pain during the surgery. You may be awake while the surgery is done.
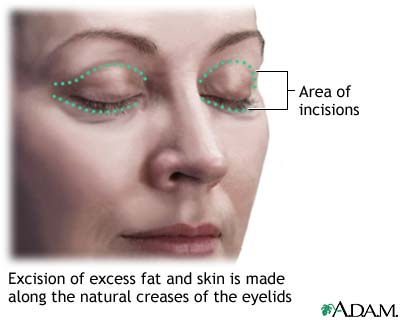
- The surgeon makes tiny cuts (incisions) into the natural creases or folds of the eyelids.
- Loose skin and extra fat tissue are removed. The eyelid muscles are then tightened if a ptosis repair is also performed.
- At the end of surgery, the incisions are closed with stitches.
Why the Procedure Is Performed
An eyelid lift is needed when eyelid drooping reduces your vision. You may be asked to have your eye doctor test your vision before you have the surgery.
Some people have an eyelid lift to improve their appearance. This is cosmetic surgery. The eyelid lift may be done alone or with other surgery such as a browlift or facelift.
Eyelid surgery will not remove wrinkles around the eyes, lift sagging eyebrows, or get rid of dark circles under the eyes.
Risks
Risks for anesthesia and surgery in general include:
- Reactions to medicines
- Bleeding, blood clots, infection
Risks for an eyelid lift may include:
- Damage to eye or loss of vision (rare)
- Difficulty closing the eyes while sleeping (rarely permanent)
- Double or blurred vision
- Dry eyes
- Temporary swelling of the eyelids
- Tiny whiteheads after stitches are removed
- Slow healing
- Uneven healing or scarring
- Eyelids may not match
Medical conditions that make blepharoplasty more risky are:
- Diabetes
- Dry eye or not enough tear production
- Heart disease or disorders of the blood vessels
- High blood pressure or other circulatory disorders
- Thyroid problems, such as hypothyroidism and Graves disease
After the Procedure
You can usually go home the day of surgery. Arrange ahead of time for an adult to drive you home.
Before you leave, the health care provider will cover your eyes and eyelids with ointment and a bandage. Your eyelids may feel tight and sore as the numbing medicine wears off. The discomfort is easily controlled often with over-the-counter pain medicine.
Keep your head raised as much as possible for several days. Place cold packs over the area to reduce swelling and bruising. Wrap the cold pack in a towel before applying. This helps prevent cold injury to the eyes and skin.
Your surgeon may recommend an antibiotic or lubricating eye drops to reduce burning or itching.
You should be able to see well after 2 to 3 days. Do not wear contact lenses for at least 2 weeks. Keep activities to a minimum for 3 to 5 days, and avoid strenuous activities that raise the blood pressure for about 3 weeks. This includes lifting, bending, and rigorous sports.
Your surgeon will remove the stitches 5 to 7 days after surgery if they need to be removed. You will have some bruising, which may last 2 to 4 weeks. You may notice increased tears, more sensitivity to light and wind, and blurring or double vision for the first few weeks.
Outlook (Prognosis)
Scars may remain slightly pink for 6 months or more after surgery. They will fade to a thin, nearly invisible white line and are hidden within the natural eyelid fold. The more alert and youthful look usually lasts for years. These results are permanent for some people.
References
Few J, Ellis M. Blepharoplasty. In: Rubin JP, Neligan PC, eds. Plastic Surgery, Volume 2: Aesthetic Surgery. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 9.
Salmon JF. Eyelids. In: Bowling B, ed. Kanski's Clinical Ophthalmology. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 2.
Review Date: 3/2/2023
Reviewed By: Tang Ho, MD, Associate Professor, Division of Facial Plastic and Reconstructive Surgery, Department of Otolaryngology – Head and Neck Surgery, The University of Texas Medical School at Houston, Houston, TX. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.