Corneal transplant
Keratoplasty; Penetrating keratoplasty; Lamellar keratoplasty; Keratoconus - corneal transplant; Fuchs' dystrophy - corneal transplant
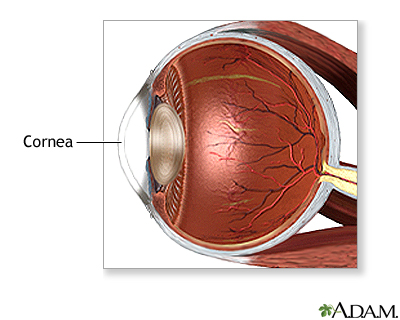
The cornea is the clear outer lens on the front of the eye. A corneal transplant is surgery to replace the cornea with tissue from a donor. It is one of the most common transplants done.
Description
You will most likely be awake during the transplant. You will get medicine to relax you. Local anesthesia (numbing medicine) will be injected around your eye to block pain and prevent eye movement during the surgery.
The tissue for your corneal transplant will come from a person (donor) who has recently died. The donated cornea is processed and tested by a local eye bank to make sure it is safe for use in your surgery.
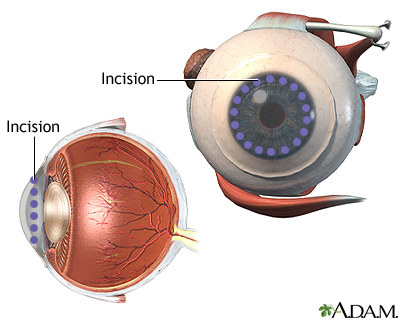
For years, the most common type of corneal transplant was called penetrating keratoplasty.
- It is still a frequently performed operation.
- During this procedure, your surgeon will remove a small round piece of your cornea.
- The donated tissue will then be sewn into the opening of your cornea.
A newer technique is called lamellar keratoplasty.
- In this procedure, only the inner or outer layers of the cornea are replaced, rather than all the layers, as in penetrating keratoplasty.
- There are several different lamellar techniques. They differ mostly on which layer is replaced and how the donor tissue is prepared.
- All lamellar procedures lead to faster recovery and fewer complications.
Why the Procedure Is Performed
A corneal transplant is recommended for people who have:
- Vision problems caused by thinning of the cornea, most often due to keratoconus. (A transplant may be considered when less invasive treatments are not an option.)
- Scarring of the cornea from severe infections or injuries
- Vision loss caused by cloudiness of the cornea, most often due to Fuchs dystrophy
Risks
The body may reject the transplanted tissue. This occurs in about 1 out of 3 patients in the first 5 years. Rejection can sometimes be controlled with steroid eye drops. There have rare cases of graft rejection reported soon after COVID-19 vaccination.
Other risks for a corneal transplant are:
- Bleeding
- Cataracts
- Infection of the eye
- Glaucoma (high pressure in the eye that can cause vision loss)
- Loss of vision
- Scarring of the eye
- Swelling of the cornea
Before the Procedure
Tell your health care provider about any medical conditions you may have, including allergies. Also tell your provider what medicines you are taking, even drugs, supplements, and herbs you bought without a prescription.
You may need to limit medicines that make it hard for your blood to clot (blood thinners) for 10 days before the surgery. Some of these are aspirin, ibuprofen (Advil, Motrin), and warfarin (Coumadin).
Ask your provider which of your other daily medicines, such as water pills, insulin or pills for diabetes, you should take on the morning of your surgery.
You will need to stop eating and drinking most fluids after midnight the night before your surgery. Most providers will let you have water, apple juice, and plain coffee or tea (without cream or sugar) up to 2 hours before surgery. Do not drink alcohol 24 hours before or after surgery.
On the day of your surgery, wear loose, comfortable clothing. Do not wear any jewelry. Do not put creams, lotions, or makeup on your face or around your eyes.
You will need to have someone drive you home after your surgery.
Note: These are general guidelines. Your surgeon may give you other instructions.
After the Procedure
You will go home on the same day as your surgery. Your provider will give you an eye patch to wear for about 1 to 4 days.
Your provider will prescribe eye drops to help your eye heal and prevent infection and rejection.
Your provider will remove the stitches at a follow-up visit. Some stitches may stay in place for as long as a year, or they might not be removed at all.
Outlook (Prognosis)
Full recovery of eyesight may take up to a year. This is because it takes time for the swelling to go down. Most people who have a successful corneal transplant will have good vision for many years. If you have other eye problems, you may still have vision loss from those conditions.
You may need glasses or contact lenses to achieve the best vision. Laser vision correction may be an option if you have nearsightedness, farsightedness, or astigmatism after the transplant has fully healed.
References
Cioffi GA, Liebmann JM. Diseases of the visual system. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 395.
Gibbons A, Sayed-Ahmed IO, Mercado CL, Chang VS, Karp CL. Corneal surgery. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 4.27.
Gómez-Benlloch A, Montesel A, Pareja-Aricò L, et al. Causes of corneal transplant failure: a multicentric study. Acta Ophthalmol. 2021;99(6):e922-e928. PMID: 33421330 pubmed.ncbi.nlm.nih.gov/33421330/.
McTiernan CD, Simpson FC, Haagdorens M, et al. LiQD cornea: pro-regeneration collagen mimetics as patches and alternatives to corneal transplantation. Science Advances. 2020;6(25):eaba2187 PMID: 32917640 pubmed.ncbi.nlm.nih.gov/32917640/.
Phylactou M, Li JO, Larkin DFP. Characteristics of endothelial corneal transplant rejection following immunisation with SARS-CoV-2 messenger RNA vaccine. Br J Ophthalmol. 2021;105(7):893-896. PMID: 33910885 pubmed.ncbi.nlm.nih.gov/33910885/.
Shah KJ, Holland EJ, Mannis MJ. Corneal transplantation in ocular surface disease. In: Mannis MJ, Holland EJ, eds. Cornea. 4th ed. Philadelphia, PA: Elsevier; 2017:chap 160.
Review Date: 8/22/2022
Reviewed By: Franklin W. Lusby, MD, Ophthalmologist, Lusby Vision Institute, La Jolla, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.