Endotracheal intubation
Intubation - endotracheal
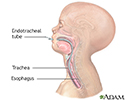
Endotracheal intubation is a medical procedure in which a tube is placed into the windpipe (trachea) through the mouth or nose. In most emergency situations, it is placed through the mouth.
Description
Whether you are awake (conscious) or not awake (unconscious), you will be given medicine to make it easier and more comfortable to insert the tube. You may also receive medicine to relax.
The health care provider will insert a device called a laryngoscope to be able to view the vocal cords and the upper part of the windpipe.
If the procedure is being done to help with breathing, a tube is then inserted into the windpipe and past the vocal cords to just above the spot where the trachea branches into the lungs. The tube can then be connected to a mechanical ventilator to assist breathing.
Why the Procedure Is Performed
Endotracheal intubation is done to:
- Keep the airway open in order to give oxygen, medicine, or anesthesia.
- Support breathing in certain illnesses, such as pneumonia, emphysema, heart failure, collapsed lung or severe trauma.
- Remove blockages from the airway.
- Allow the provider to get a better view of the upper airway.
- Protect the lungs in people who are unable to protect their airway and are at risk for breathing in fluid (aspiration). This includes people with certain types of strokes, overdoses, or massive bleeding from the esophagus or stomach.
Risks
Risks include:
- Bleeding
- Infection
- Trauma to the voice box (larynx), thyroid gland, vocal cords and windpipe (trachea), or esophagus
- Puncture or tearing (perforation) of body parts in the chest cavity, leading to lung collapse
Before the Procedure
The procedure is most often done in emergency situations, so there are no steps you can take to prepare.
After the Procedure
You will be in the hospital to monitor your breathing and your blood oxygen levels. You may be given oxygen or placed on a breathing machine. If you are awake, your provider may give you medicine to reduce your anxiety or discomfort.
Outlook (Prognosis)
The outlook will depend on the reason the procedure needed to be done.
References
Casey DF. Tracheal intubation. In: Fowler GC, ed. Pfenninger and Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 222.
Driver BE, Reardon RF. Tracheal intubation. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges' Clinical Procedures in Emergency Medicine and Acute Care. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 4.
Hartman ME, Cheifetz IM. Pediatric emergencies and resuscitation. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 81.
Review Date: 10/6/2022
Reviewed By: Jesse Borke, MD, CPE, FAAEM, FACEP, Attending Physician at Kaiser Permanente, Orange County, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.