Testicular self-exam
Screening - testicular cancer - self-exam; Testicular cancer - screening - self-exam
Testicular self-exam is an examination of the testicles that you do on yourself.
How the Test is Performed
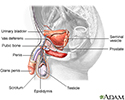
The testicles (also called the testes) are the male reproductive organs that produce sperm and the hormone testosterone. They are located in the scrotum under the penis.
You can do this test during or after a shower. This way, the scrotal skin is warm and relaxed. It is best to do the test while standing.
- Gently feel your scrotal sac to locate a testicle.
- Use one hand to stabilize the testicle. Use your fingers and thumb of the other hand to firmly but gently feel the testicle. Feel the entire surface.
- Check the other testicle in the same way.
Why the Test is Performed
A testicular self-exam is done to check for testicular cancer.
Testicles have blood vessels and other structures that can make the exam confusing. If you notice any lumps or changes in a testicle, contact your health care provider right away.
Your provider may recommend that you do a testicular self-exam every month if you have any of the following risk factors:
- Family history of testicular cancer
- Past testicular tumor
- Undescended testicle
However, if a man has no risk factors or symptoms, experts do not know if doing testicular self-exam lowers the chance of dying of this cancer. The US Preventive Services Task Force recommends against testicular exams in men with no symptoms and no risk factors for testicular cancer.
Normal Results
Each testicle should feel firm, but not rock hard. One testicle may be lower or slightly larger than the other.
Talk to your provider if you have questions.
What Abnormal Results Mean
If you find a small, hard lump (like a pea), have an enlarged testicle, or notice any other differences that do not seem normal, see your provider right away.
Contact your provider if:
- You cannot find one or both testicles. The testicles may not have descended properly in the scrotum.
- There is a soft collection of thin tubes above the testicle. This may be a collection of widened veins (varicocele).
- You have pain or swelling in the scrotum. This may be an infection or a fluid-filled sac (hydrocele) causing a blockage of blood flow to the area. It may be difficult to feel the testicle if there is fluid in the scrotum.
Sudden, severe (acute) pain in the scrotum or testicle that lasts for more than a few minutes is an emergency. If you have this type of pain, seek medical attention right away.
A lump in the testicle is often the first sign of testicular cancer. If you find a lump, see a provider right away. Most testicular cancers are very treatable. Keep in mind that some cases of testicular cancer do not show symptoms until they reach an advanced stage.
Risks
There are no risks with this self-exam.
References
American Cancer Society website. Can testicular cancer be found early? www.cancer.org/cancer/testicular-cancer/detection-diagnosis-staging/detection.html. Updated May 17, 2018. Accessed July 18, 2023.
Friedlander TW, Small E. Testicular cancer. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 83.
National Cancer Institute website. Testicular cancer screening (PDQ) - health professional version. www.cancer.gov/types/testicular/hp/testicular-screening-pdq. Updated April 28, 2023. Accessed July 18, 2023.
US Preventive Services Task Force. Screening for testicular cancer: US Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2011;154(7):483-486. PMID: 21464350 pubmed.ncbi.nlm.nih.gov/21464350/.
Review Date: 7/1/2023