Hypersensitivity pneumonitis
Extrinsic allergic alveolitis; Farmer's lung; Mushroom picker's disease; Humidifier or air-conditioner lung; Bird breeder's or bird fancier's lung
Hypersensitivity pneumonitis is inflammation of the lungs due to breathing in dust, fungus, molds, or other substances.
Causes
Hypersensitivity pneumonitis usually occurs in people who work in places where there are high levels of dust, fungus, or molds.
Long-term exposure can lead to lung inflammation and acute lung disease. Over time, the acute condition turns into long-lasting (chronic) lung disease.
Hypersensitivity pneumonitis may also be caused by:
- Fungi or bacteria in humidifiers, heating systems, and air conditioners found in homes and offices
- Exposure to certain chemicals, such as isocyanates or acid anhydrides
Examples of hypersensitivity pneumonitis include:
Bird fancier's lung is caused by exposure to proteins found in the feathers or droppings of many species of birds. This is the most common type of hypersensitivity pneumonitis.
Farmer's lung is caused by exposure to dust from moldy hay, straw, and grain.
Symptoms
Symptoms often occur 4 to 8 hours after you have left the area where the triggering substance is found. This makes it hard to figure out what has caused the disease. Your symptoms may get better before you go back to the area where you were exposed to the substance. In the chronic phase of the condition, the symptoms are more constant and less affected by exposure to the substance.
Symptoms after acute exposure may include:
- Chills
- Cough
- Fever
- Malaise (feeling ill)
- Shortness of breath
Symptoms of chronic hypersensitivity pneumonitis may include:
- Breathlessness, especially with activity
- Cough, often dry
- Loss of appetite
- Unintentional weight loss
Exams and Tests
Your health care provider will perform a physical examination and ask about your symptoms.
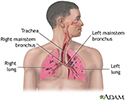
Your provider may hear abnormal lung sounds called crackles (rales) when listening to your chest with a stethoscope.
Lung changes due to chronic hypersensitivity pneumonitis may be seen on a chest x-ray. Other tests may include:
- Aspergillosis precipitin blood test to check if you've been exposed to the aspergillus fungus
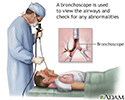
- Bronchoscopy with washings, biopsy, and bronchoalveolar lavage
- Complete blood count (CBC)
- CT scan of the chest
- Hypersensitivity pneumonitis antibody panel blood test
- Krebs von den Lungen-6 assay (KL-6) blood test
- Lung function tests
- Surgical lung biopsy
Treatment
First, the offending substance must be identified. Treatment involves avoiding this substance in the future. Some people may need to change jobs if they cannot avoid the substance at work.
If you have a chronic form of this disease, your provider may recommend that you take glucocorticoids (anti-inflammatory medicines). Sometimes, treatments used for asthma can help people with hypersensitivity pneumonitis. Sometimes medicines that suppress the immune system are needed to control the disease.
Outlook (Prognosis)
Most symptoms go away when you avoid or limit your exposure to the material that caused the problem. The outlook is good if you prevent exposure during the acute stage. When it reaches the chronic stage, the disease might continue to progress, even if the offending substance is avoided.
Possible Complications
The chronic form of this disease may lead to pulmonary fibrosis. This is scarring of the lung tissue that often is not reversible. Eventually, end-stage lung disease and respiratory failure can occur. Some people might need lung transplantation at the end-stage of the disease.
When to Contact a Medical Professional
Contact your provider if you develop symptoms of hypersensitivity pneumonitis, especially if you have been exposed to potentially harmful agents that can cause the disease.
Prevention
The chronic form can be prevented by avoiding the material that causes the lung inflammation.
References
Johannson KA, Fernandez Perez ER. Hypersensitivity pneumonitis. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 91.
Tarlo SM. Occupational lung disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 87.
Review Date: 5/3/2023
Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron, Jr. Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.